There are myriad treatment options for back pain caused by lumbar degenerative disc disease, and it is common for several treatments to be combined to achieve both near-term pain relief and longer-term rehabilitation.
Most people with degenerative disc disease respond well to nonsurgical treatments.
- Research indicates that 90% of patients report improvement in back pain and radicular leg pain within 3 months of nonsurgical treatments.1Donnally III CJ, Hanna A, Varacallo M. Lumbar Degenerative Disk Disease. In: StatPearls. Treasure Island (FL): StatPearls Publishing; February 9, 2021.
- Surgical intervention may be extensive, so most people are well-served making a concerted effort with nonsurgical treatment regimens.
The long-term outlook for this condition is usually favorable, especially when coupled with lifestyle modifications and the correct use of ergonomics.1Donnally III CJ, Hanna A, Varacallo M. Lumbar Degenerative Disk Disease. In: StatPearls. Treasure Island (FL): StatPearls Publishing; February 9, 2021.
This article describes the various treatments available to manage the symptoms of degenerative disc disease, including addressing both painful flare-ups as well as longer-term pain management and rehabilitation.
In This Article:
- Degenerative Disc Disease Treatment for Low Back Pain
- Exercise and Physical Therapy for Disc Disease Treatment and Pain Management
- Pain Medications for Degenerative Disc Disease Treatment
- Pain Management Techniques for Degenerative Disc Disease
- Treating Chronic Pain and Depression from Degenerative Disc Disease
Degenerative Disc Disease Treatment Goals
The vast majority of people with degenerative disc disease experience low back pain symptoms that flare up periodically, but do not get worse over time. For those people, the main goals for managing lower back pain caused by degenerative disc disease are usually:
- Achieving enough pain relief to be able to engage in lower back pain exercises and a rehabilitation program
- Trying to manage the low back pain and maintaining an ability to function at home and at work.
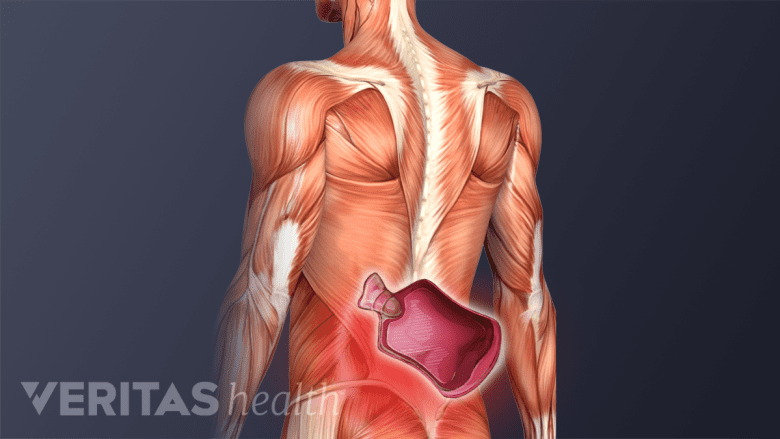
Once a disc has degenerated, the degenerative process cannot be reversed. Instead of trying to rehabilitate the disc itself, treatment focuses on improving the health of surrounding structures, such as the spinal nerves, vertebral bones and joints, and supporting muscles and ligaments.
See The "Degenerative Cascade" of a Degenerating Disc
The main goals of the rehabilitation program include a therapist-guided and individual approach, which aim to2Miletic J, Gart A. Land Based Rehabilitation and the Aging Spine. In: The Comprehensive Treatment of the Aging Spine. Elsevier; 2011:99-102. doi:10.1016/b978-1-4377-0373-3.10017-x:
- Increase, restore, and/or maintain the range of motion in the affected spinal segment
- Build physical strength, flexibility, coordination, balance, and endurance in the lower back and legs
- Guide patients to make ergonomic changes in their workspace and home to support the spine and prevent recurrence of pain
- Teach the correct use of posture while sitting, walking, sleeping, and lifting to promote maximum function with lesser pain
Continuing to build overall fitness through exercise programs and teaching patients to promote maximum function and independence within their capability is usually continued for a few months after the initial treatment(s).2Miletic J, Gart A. Land Based Rehabilitation and the Aging Spine. In: The Comprehensive Treatment of the Aging Spine. Elsevier; 2011:99-102. doi:10.1016/b978-1-4377-0373-3.10017-x
Example Progression of Treatment Regimens for Lumbar Degenerative Disc Disease
NSAIDs provide anti-inflammatory effects and help calm inflammation and pain in the back.
Treatments need to be individualized. However, as a general rule, lumbar degenerative disc disease treatments start with basic pain control and non-invasive treatments and progress, if needed, to more extensive and/or invasive treatments.
One example of how treatment approaches may progress over time would be:
- Bed rest, or reduced activity, for the first 1 to 2 days after onset of severe pain, combined with anti-inflammatory medication such as ibuprofen, and ice and/or heat therapy
- Prescription muscle relaxant medications, as needed, for up to 1 week
- Gentle stretching and aerobic exercise, for at least 3 times a week
- Physical therapy if after 3 weeks there is no improvement in pain
- An epidural injection if after 3 to 6 weeks there is little to no improvement in pain
- Spinal surgery if after 6 to 12 months the pain is severe, ongoing and significantly limits daily activities
Bed rest beyond the first 2 days of sharp, severe pain is not usually advised, because regular movement improves blood circulation and muscle strength and helps the body to heal more quickly than bed rest.
The above is just one example of a typical progression of treatments, and additional therapies or a different type of progression of care is not uncommon based on the patient’s condition and the treating physician’s preferences as well as other variables.
Active and Passive Treatment Options
Heat therapy relaxes muscles and fosters healing by improving blood flow.
The treatments for degenerative disc disease generally fall into two categories:
- Active treatments, which are performed by the patient
- Passive treatments, which are done to the patient
Passive treatments, such as pain medications or injections, are rarely effective on their own—an active component, such as a controlled, progressive exercise program for rehabilitation, is almost always recommended.
Additional therapies, such as heat therapy, acupuncture, and behavioral therapy, may also provide enough low back pain relief to allow the continuation of an exercise and rehabilitation program.
Team Approach to Pain Management
For some, an integrated team of specialists may be best suited to manage the chronic lower back pain from degenerative disc disease. A team will usually comprise some combination of the following health professionals:
- A pain management specialist, such as a physical medicine and rehabilitation physician (physiatrist) or anesthesiologist focused on pain management
- A physical therapist or physiatrist focused on rehabilitation
- A psychologist and/or psychiatrist for co-existing mental health issues, such as depression and/or difficulty sleeping
- An occupational therapist to assist with functional rehabilitation
In addition, a specialized nurse case manager or another health professional may work with the team to coordinate the care needed to treat depression, disability, and chronic pain.
Read more about Specialists Who Treat Back Pain
Sometimes the combination of treatments is more effective than individual treatments. For example, the use of cognitive behavioral therapy has been shown to improve the benefits of physical therapy3Hajihasani A, Rouhani M, Salavati M, Hedayati R, Kahlaee AH. The Influence of Cognitive Behavioral Therapy on Pain, Quality of Life, and Depression in Patients Receiving Physical Therapy for Chronic Low Back Pain: A Systematic Review. PM R. 2019;11(2):167-176. doi:10.1016/j.pmrj.2018.09.029 and reduce sleep problems.
- 1 Donnally III CJ, Hanna A, Varacallo M. Lumbar Degenerative Disk Disease. In: StatPearls. Treasure Island (FL): StatPearls Publishing; February 9, 2021.
- 2 Miletic J, Gart A. Land Based Rehabilitation and the Aging Spine. In: The Comprehensive Treatment of the Aging Spine. Elsevier; 2011:99-102. doi:10.1016/b978-1-4377-0373-3.10017-x
- 3 Hajihasani A, Rouhani M, Salavati M, Hedayati R, Kahlaee AH. The Influence of Cognitive Behavioral Therapy on Pain, Quality of Life, and Depression in Patients Receiving Physical Therapy for Chronic Low Back Pain: A Systematic Review. PM R. 2019;11(2):167-176. doi:10.1016/j.pmrj.2018.09.029