XLIF (extreme lateral interbody fusion) is a minimally invasive surgical procedure that fuses two levels of the spine using an approach from the side of the lower back. The surgery typically involves the removal of the spinal disc and placement of an interbody cage filled with bone graft in the disc space. The treated segments are then secured with fusion instrumentation, such as pedicle screws and rods.
Specifically, the abbreviation XLIF stands for:
- eXtreme, so named by the surgeons who introduced the approach
- Lateral, which means from the side of the body
- Interbody, which refers to the area between two adjacent vertebral bones in the spine
- Fusion, which refers to the process of two vertebral bones growing together
This surgery may also be referred to as Lateral Lumbar Interbody Fusion (LLIF) or Direct Lateral Interbody Fusion (DLIF).
In This Article:
- XLIF: Lumbar Spinal Fusion
- Description of XLIF Surgery
When XLIF May Be Considered
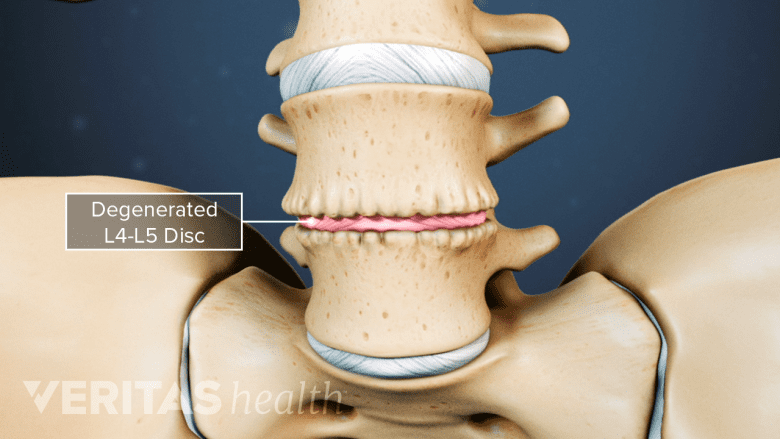
XLIF helps reduce pain and instability from degenerative disc disease.
XLIF may be used to treat lower back conditions including but not limited to:
- Lumbar degenerative disc disease
- Recurrent lumbar disc herniation
- Low-grade spondylolisthesis
- Degenerative scoliosis
- Foraminal stenosis
XLIF can be performed on a single level or multiple levels.
XLIF may also be a preferred surgical technique for patients who need a revision surgery for conditions such as failed fusion, painful implants, or post-surgical complications.1Formica M, Zanirato A, Cavagnaro L, et al. Extreme lateral interbody fusion in spinal revision surgery: clinical results and complications. Eur Spine J. 2017;26(Suppl 4):464-470. doi:10.1007/s00586-017-5115-6 In such revision surgeries, XLIF may promote better fusion and reduce the risk of nerve injuries compared to other techniques, such as posterior lumbar interbody fusion (PLIF).1Formica M, Zanirato A, Cavagnaro L, et al. Extreme lateral interbody fusion in spinal revision surgery: clinical results and complications. Eur Spine J. 2017;26(Suppl 4):464-470. doi:10.1007/s00586-017-5115-6
When XLIF Is Not an Option
Fusing L5-S1 via XLIF is difficult due to its low position and limited access.
Anatomical challenges may sometimes make the XLIF surgery difficult to perform. These challenges include but are not limited to:
- Fusion of the lowermost segments of the spine, which are hard to access from the side. These segments may include:
- The L5-S1 spinal segment, which is situated below the level of the pelvic brim
- An anatomic variant of the L4-L5 spinal segment where the segment is situated lower than usual2Smith WD, Youssef JA, Christian G, Serrano S, Hyde JA. Lumbarized sacrum as a relative contraindication for lateral transpsoas interbody fusion at L5-6. J Spinal Disord Tech. 2012;25(5):285-291. doi:10.1097/BSD.0b013e31821e262f
- High-grade spondylolisthesis, where the position of exiting nerve roots limits access to the spinal segments3Beck AW, Simpson AK. High-Grade Lumbar Spondylolisthesis. Neurosurg Clin N Am. 2019;30(3):291-298. doi:10.1016/j.nec.2019.02.002
As with any spinal fusion surgery, the patient’s underlying lower back condition is assessed through physical and diagnostic tests, and the advantages and disadvantages of surgery must be discussed in detail with the surgeon—to determine if XLIF is the surgery of choice.
Benefits of an XLIF Back Surgery
The minimally invasive approach of the XLIF procedure helps conserve more spinal tissue and minimize post-surgical discomfort. These benefits may be offered through4Berjano P, Gautschi OP, Schils F, Tessitore E. Extreme lateral interbody fusion (XLIF®): how I do it. Acta Neurochir (Wien). 2015;157(3):547-551. doi:10.1007/s00701-014-2248-9:
- Preserved longitudinal (length-wise) ligaments and muscles surrounding the spine
- Potential use of larger cage implants, which allows more surface area for bony fusion and better surgical outcomes
- Less blood loss
- Short duration of surgery
- Small incisions and scars
- Low risk of infection
Compared to other lumbar spine fusion techniques, XLIF also offers a relatively quick recovery time and return to normal function.
Variations of XLIF
The XLIF technique may be modified by approaching the spinal segment through different angles along the side of the spine with the intent of preserving spinal tissues and targeting the spinal problem. These variations include:
- Stand-alone XLIF, where an interbody cage is used without additional support from pedicle screws or rods. Stand-alone XLIF is typically not recommended in conditions that may cause post-surgical instability, such as facet joint arthritis, bone deformity, or when the adjacent segment is surgically fused.5Malham GM, Ellis NJ, Parker RM, et al. Maintenance of Segmental Lordosis and Disk Height in Stand-alone and Instrumented Extreme Lateral Interbody Fusion (XLIF). Clin Spine Surg. 2017;30(2):E90-E98. doi:10.1097/BSD.0b013e3182aa4c94 Under these conditions, a screw-rod construct is a necessary measure to help fixate the segment and support bony fusion.
- Prone single-position XLIF, where the patient lies face-down instead of on their side. Prone single-position XLIF may be considered in more complex cases, such as spinal deformity.6Lamartina C, Berjano P. Prone single-position extreme lateral interbody fusion (Pro-XLIF): preliminary results. Eur Spine J. 2020;29(Suppl 1):6-13. doi:10.1007/s00586-020-06303-z
- Oblique lumbar interbody fusion (OLIF), where an oblique approach is taken to preserve the psoas muscle in the front of the hip and the lumbosacral plexus (a group of nerve fibers derived from the lumbar spinal nerves).7Woods KR, Billys JB, Hynes RA. Technical description of oblique lateral interbody fusion at L1-L5 (OLIF25) and at L5-S1 (OLIF51) and evaluation of complication and fusion rates. Spine J. 2017;17(4):545-553. doi:10.1016/j.spinee.2016.10.026 In addition to the L1-L5 levels of the lumbar spine, the OLIF technique also allows a surgeon to treat the lowermost L5-S1 spinal segment, which usually cannot be accessed through traditional XLIF.8Woods KR, Billys JB, Hynes RA. Technical description of oblique lateral interbody fusion at L1-L5 (OLIF25) and at L5-S1 (OLIF51) and evaluation of complication and fusion rates. Spine J. 2017;17(4):545-553. doi:10.1016/j.spinee.2016.10.026
In general, these variations have similar surgical outcomes and success rates compared to standard XLIF.1Formica M, Zanirato A, Cavagnaro L, et al. Extreme lateral interbody fusion in spinal revision surgery: clinical results and complications. Eur Spine J. 2017;26(Suppl 4):464-470. doi:10.1007/s00586-017-5115-6,9Li HM, Zhang RJ, Shen CL. Differences in radiographic and clinical outcomes of oblique lateral interbody fusion and lateral lumbar interbody fusion for degenerative lumbar disease: a meta-analysis. BMC Musculoskelet Disord. 2019;20(1):582. Published 2019 Dec 4. doi:10.1186/s12891-019-2972-7,10Hah R, Kang HP. Lateral and Oblique Lumbar Interbody Fusion-Current Concepts and a Review of Recent Literature [published online ahead of print, 2019 Jun 22]. Curr Rev Musculoskelet Med. 2019;12(3):305-310. doi:10.1007/s12178-019-09562-6
How XLIF Compares with Other Spine Fusion Surgeries
The type of spine fusion surgery typically depends on the condition being treated, overall health of the patient, skill of the surgeon, and presence of any contraindications that may rule out a specific procedure. While all types of interbody fusion surgeries serve the same purpose of fusing two spinal segments, the XLIF technique may offer a few potential advantages due to its minimally invasive approach.
XLIF vs ALIF
ALIF accesses the spine through the abdomen.
The XLIF technique approaches the spine through an incision made on the side of the lower back. An anterior lumbar interbody fusion (ALIF) approach is from the front, through the abdomen, and requires the organs in the abdomen and some of the major blood vessels to be moved to the side so that the surgeon can reach the spine.11Laratta JL, Davis EG, Glassman SD, Dimar JR. The transperitoneal approach for anterior lumbar interbody fusion at L5-S1: a technical note. J Spine Surg. 2018;4(2):459-460. doi:10.21037/jss.2018.05.18
In order to minimize the risk of blood vessel and/or organ injury, a vascular surgeon or general surgeon usually performs the first part of the ALIF surgery. In an XLIF procedure, the approach from the side does not require any major organs or blood vessels to be moved.
Watch ALIF (Anterior Lumbar Interbody Fusion) Video
XLIF vs PLIF
With the XLIF approach from the side, only the lateral (side) muscles are separated along their fibers and there is no cutting or tearing of the muscle. A posterior lumbar interbody fusion (PLIF) surgery approaches the spine from the back and requires some of the major muscles to be cut to access the spinal segment.
Research suggests that XLIF may restore more disc height compared to the PLIF approach.12Mobbs RJ, Phan K, Malham G, Seex K, Rao PJ. Lumbar interbody fusion: techniques, indications and comparison of interbody fusion options including PLIF, TLIF, MI-TLIF, OLIF/ATP, LLIF and ALIF. J Spine Surg. 2015;1(1):2-18. doi:10.3978/j.issn.2414-469X.2015.10.05
Watch Posterior Lumbar Interbody Fusion (PLIF) Video
XLIF vs TLIF
Transforaminal lumbar interbody fusion (TLIF) approaches the spine from the back and is similar to posterior lumbar interbody fusion (PLIF), also requiring major muscles to be cut to access the spinal segment. While XLIF indirectly decompresses the nerves by restoring disc height, TLIF directly decompresses neural tissues by widening the bony openings or foramina.13Guigui P, Ferrero E. Surgical treatment of degenerative spondylolisthesis. Orthop Traumatol Surg Res. 2017;103(1S):S11-S20. doi:10.1016/j.otsr.2016.06.022
Both XLIF and TLIF are newer approaches to spinal fusion that are still being developed and studied for their advantages and drawbacks, compared to more traditional approaches.
Potential Risks and Complications of XLIF Back Surgery
Damage to the lumbar spinal nerves is a potential risk of XLIF surgery.
The XLIF approach may give rise to potential complications, which are typically more likely to occur in patients who are obese or have ongoing health conditions, such as diabetes. The specific spinal segment being treated and the vital structures in its proximity may also contribute to the potential risks.
Pseudoarthrosis
The primary potential complication of an XLIF surgery is failure to fuse or non-union of the joint, also called pseudoarthrosis. Pseudoarthrosis may go undetected or lead to a recurrence of pain.14Jung JM, Chung CK, Kim CH, Yang SH, Ko YS. Prognosis of Symptomatic Pseudarthrosis Observed at 1 Year After Lateral Lumbar Interbody Fusion. Spine (Phila Pa 1976). 2021;46(18):E1006-E1013. doi:10.1097/BRS.0000000000003980 In most cases, the pain typically resolves without treatment in about 88% of these patients by the second year after surgery.10Hah R, Kang HP. Lateral and Oblique Lumbar Interbody Fusion-Current Concepts and a Review of Recent Literature [published online ahead of print, 2019 Jun 22]. Curr Rev Musculoskelet Med. 2019;12(3):305-310. doi:10.1007/s12178-019-09562-6
Diabetes and smoking are possible risk factors that may explain some cases of symptomatic pseudoarthrosis that continue beyond 2 years, which may require additional surgery to relieve pain.4Berjano P, Gautschi OP, Schils F, Tessitore E. Extreme lateral interbody fusion (XLIF®): how I do it. Acta Neurochir (Wien). 2015;157(3):547-551. doi:10.1007/s00701-014-2248-9
Nerve damage
Another potential complication of XLIF is damage to the spinal nerves or spinal cord. The retractor used for XLIF places pressure on the nerves running through the iliopsoas muscle in the lower spine and pelvis, leading to the potential risk of neural compromise. The damage can result in thigh pain or weakness in the thigh muscles (quadriceps).
This risk is mainly dependent on the patient’s overall build, the location of the fusion, and the surgeon’s experience in this procedure. Nerve injuries during an XLIF procedure can be reduced by intraoperative nerve monitoring, where an additional provider will track nerve signals during the surgery.15Epstein NE. Many Intraoperative Monitoring Modalities Have Been Developed To Limit Injury During Extreme Lateral Interbody Fusion (XLIF/MIS XLIF): Does That Mean XLIF/MIS XLIF Are Unsafe?. Surg Neurol Int. 2019;10:233. Published 2019 Nov 29. doi:10.25259/SNI_563_2019
Other possible complications associated with XLIF include but are not limited to infection, muscle weakness, pneumonia, worsening of symptoms, and accelerated degeneration at neighboring spinal levels, medically known as adjacent segment disease. As with any surgical procedure, a discussion detailing all the potential risks of the XLIF procedure should take place between the physician and the patient.
- 1 Formica M, Zanirato A, Cavagnaro L, et al. Extreme lateral interbody fusion in spinal revision surgery: clinical results and complications. Eur Spine J. 2017;26(Suppl 4):464-470. doi:10.1007/s00586-017-5115-6
- 2 Smith WD, Youssef JA, Christian G, Serrano S, Hyde JA. Lumbarized sacrum as a relative contraindication for lateral transpsoas interbody fusion at L5-6. J Spinal Disord Tech. 2012;25(5):285-291. doi:10.1097/BSD.0b013e31821e262f
- 3 Beck AW, Simpson AK. High-Grade Lumbar Spondylolisthesis. Neurosurg Clin N Am. 2019;30(3):291-298. doi:10.1016/j.nec.2019.02.002
- 4 Berjano P, Gautschi OP, Schils F, Tessitore E. Extreme lateral interbody fusion (XLIF®): how I do it. Acta Neurochir (Wien). 2015;157(3):547-551. doi:10.1007/s00701-014-2248-9
- 5 Malham GM, Ellis NJ, Parker RM, et al. Maintenance of Segmental Lordosis and Disk Height in Stand-alone and Instrumented Extreme Lateral Interbody Fusion (XLIF). Clin Spine Surg. 2017;30(2):E90-E98. doi:10.1097/BSD.0b013e3182aa4c94
- 6 Lamartina C, Berjano P. Prone single-position extreme lateral interbody fusion (Pro-XLIF): preliminary results. Eur Spine J. 2020;29(Suppl 1):6-13. doi:10.1007/s00586-020-06303-z
- 7 Woods KR, Billys JB, Hynes RA. Technical description of oblique lateral interbody fusion at L1-L5 (OLIF25) and at L5-S1 (OLIF51) and evaluation of complication and fusion rates. Spine J. 2017;17(4):545-553. doi:10.1016/j.spinee.2016.10.026
- 8 Woods KR, Billys JB, Hynes RA. Technical description of oblique lateral interbody fusion at L1-L5 (OLIF25) and at L5-S1 (OLIF51) and evaluation of complication and fusion rates. Spine J. 2017;17(4):545-553. doi:10.1016/j.spinee.2016.10.026
- 9 Li HM, Zhang RJ, Shen CL. Differences in radiographic and clinical outcomes of oblique lateral interbody fusion and lateral lumbar interbody fusion for degenerative lumbar disease: a meta-analysis. BMC Musculoskelet Disord. 2019;20(1):582. Published 2019 Dec 4. doi:10.1186/s12891-019-2972-7
- 10 Hah R, Kang HP. Lateral and Oblique Lumbar Interbody Fusion-Current Concepts and a Review of Recent Literature [published online ahead of print, 2019 Jun 22]. Curr Rev Musculoskelet Med. 2019;12(3):305-310. doi:10.1007/s12178-019-09562-6
- 11 Laratta JL, Davis EG, Glassman SD, Dimar JR. The transperitoneal approach for anterior lumbar interbody fusion at L5-S1: a technical note. J Spine Surg. 2018;4(2):459-460. doi:10.21037/jss.2018.05.18
- 12 Mobbs RJ, Phan K, Malham G, Seex K, Rao PJ. Lumbar interbody fusion: techniques, indications and comparison of interbody fusion options including PLIF, TLIF, MI-TLIF, OLIF/ATP, LLIF and ALIF. J Spine Surg. 2015;1(1):2-18. doi:10.3978/j.issn.2414-469X.2015.10.05
- 13 Guigui P, Ferrero E. Surgical treatment of degenerative spondylolisthesis. Orthop Traumatol Surg Res. 2017;103(1S):S11-S20. doi:10.1016/j.otsr.2016.06.022
- 14 Jung JM, Chung CK, Kim CH, Yang SH, Ko YS. Prognosis of Symptomatic Pseudarthrosis Observed at 1 Year After Lateral Lumbar Interbody Fusion. Spine (Phila Pa 1976). 2021;46(18):E1006-E1013. doi:10.1097/BRS.0000000000003980
- 15 Epstein NE. Many Intraoperative Monitoring Modalities Have Been Developed To Limit Injury During Extreme Lateral Interbody Fusion (XLIF/MIS XLIF): Does That Mean XLIF/MIS XLIF Are Unsafe?. Surg Neurol Int. 2019;10:233. Published 2019 Nov 29. doi:10.25259/SNI_563_2019