The aorta is the body’s main artery that stretches from the heart and down through the abdomen. When it weakens or balloons in size, the condition is known as an aortic aneurysm. This condition can cause significant abdominal pain and back pain and may lead to the artery’s leak or rupture, at which point it becomes a life-threatening emergency.
See When Back Pain May Be a Medical Emergency
An aortic enlargement occurs when the arterial walls are weakened, and is considered an aneurysm when the artery grows to at least 1 or 1.5 times its original size, or 3 cm in diameter for the abdominal aorta.1Aggarwal S, Qamar A, Sharma V, Sharma A. Abdominal aortic aneurysm: A comprehensive review. Experimental & Clinical Cardiology. 2011;16(1):11-15.
In the elderly population, abdominal aortic aneurysms are not uncommon and are rarely symptomatic. Abdominal aneurysms are most common after age 65, and are more prevalent among men and those who smoke cigarettes.2Fact Sheet: Abdominal Aortic Aneurysm. Center for Disease Control and Prevention Website. Updated June 16, 2016. Accessed October 15, 2016.
In This Article:
- Abdominal Aortic Aneurysm
- Abdominal Aortic Aneurysm Symptoms
- Abdominal Aortic Aneurysm Causes
- Abdominal Aortic Aneurysm Treatment
Function of the Abdominal Aorta
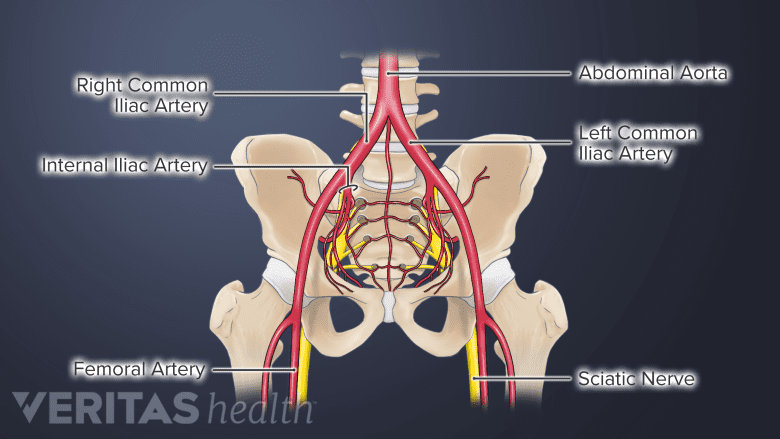
The abdominal aorta lies deep within the abdomen, positioned in front of the spine.
The aorta is the main artery that transports blood away from the heart to deliver it throughout the body, moving blood directly down through the chest and abdomen. All along the aorta are smaller arteries branching off to the various organs and systems of the body.
The abdominal aorta is the portion of the artery that sits deep in the abdomen below the kidneys and near the front of the spine. Because the aorta is near the lower spine, sudden intense pain that is felt in the lower back is a common symptom.
See Lumbar Spine Anatomy and Pain
Aortic aneurysms are most common in the abdominal aorta, with some estimates suggesting as many as 80% of aortic aneurysms occur in the abdomen.1Aggarwal S, Qamar A, Sharma V, Sharma A. Abdominal aortic aneurysm: A comprehensive review. Experimental & Clinical Cardiology. 2011;16(1):11-15.
Rupture of an Abdominal Aortic Aneurysm
The rupture of an abdominal aorta may lead to internal bleeding.
The weakened aorta may develop a leak, called a rupture, or blood may pool up between layers in the arterial walls and quickly lead to rupture, called a dissection. Internal bleeding caused by a ruptured aorta is the primary complication from an abdominal aortic aneurysm.
The loss of blood from aortic rupture is considered a catastrophic and potentially fatal medical emergency; the mortality rate for this condition increases significantly when the artery leaks. There are few ways of forecasting when an abdominal aortic aneurysm will rupture, making the condition important to detect, monitor, and manage when possible.
An aneurysm’s risk for rupture is typically dependent on the following factors:
- Size of aneurysm. Abdominal aortic aneurysms that are smaller than 5 cm in diameter tend to be considered a low risk for rupture, while aneurysms larger than 5 cm in diameter are typically considered a high risk. An aneurysm’s size tends to be the best predictor for its chance of rupturing.
- Rate of growth. Aneurysms that expand by more than half a centimeter over 6 months of regular monitoring are considered fast-growing and high risk.1Aggarwal S, Qamar A, Sharma V, Sharma A. Abdominal aortic aneurysm: A comprehensive review. Experimental & Clinical Cardiology. 2011;16(1):11-15. Aneurysm growth tends to be faster in people who smoke or have high blood pressure.
Abdominal aortic aneurysms generally do not produce severe abdominal and/or lower back pain or other symptoms until the artery has ruptured. In some cases, if an abdominal aortic aneurysm has significantly expanded it may cause symptoms similar to a rupture.