People with severe, chronic back pain know how it can utterly disrupt and damage one’s life. Chronic back pain can be cruel—making it hard to enjoy even the simplest daily activities or carry out an exercise routine.
In This Article:
- Chronic Pain As a Disease: Why Does It Still Hurt?
- Types of Back Pain: Acute Pain, Chronic Pain, and Neuropathic Pain
- When Acute Pain Becomes Chronic Pain
- Understanding Chronic Pain
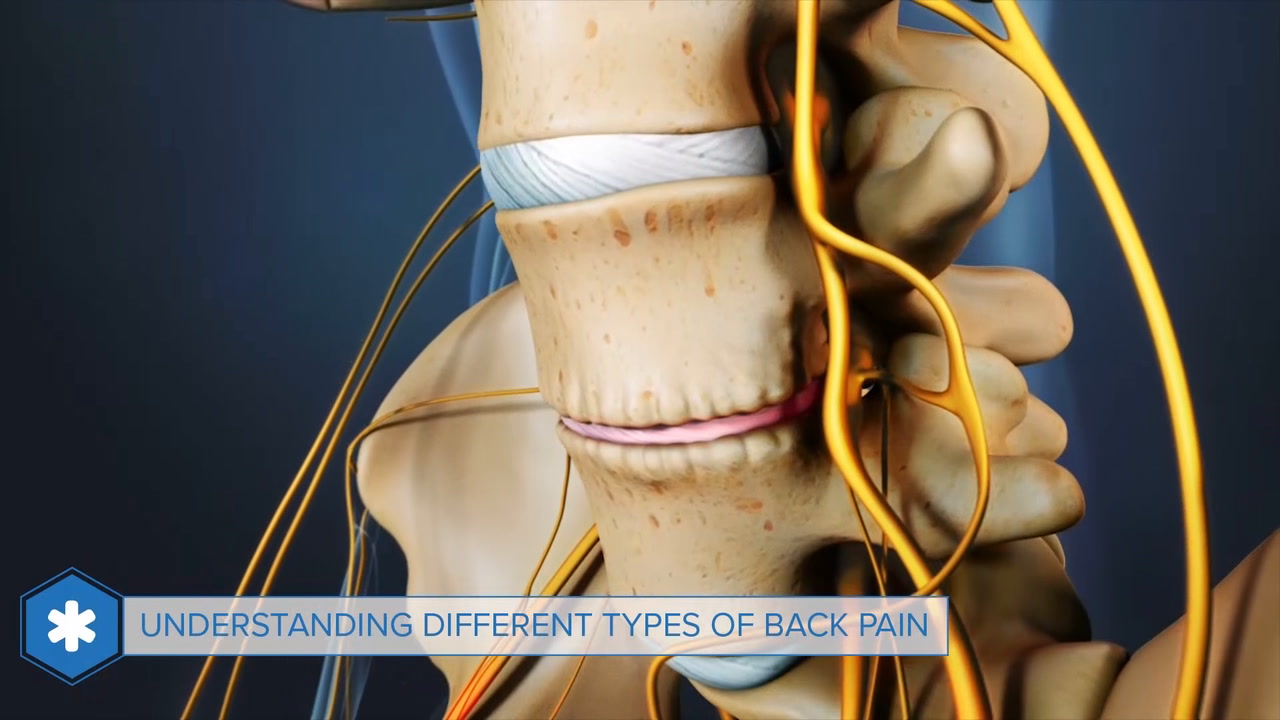
Understanding Chronic Back Pain
Despite the toll chronic pain takes—surveys estimate that 11 to 40 percent of Americans are dealing with chronic pain1Johannes C, et al. The Prevalence of Chronic Pain in United States Adults: Results of an Internet-Based Survey. J Pain. 2010 November; 11(11): 1230–1239, as cited in the National Pain Strategy: A Comprehensive Population Health-Level Strategy for Pain, United States Department of Health and Human Services, iprcc.nih.gov/National_Pain_Strategy/NPS_Main.htm.,2Nahin, R. 2015 Estimates of Pain Prevalence and Severity in Adults: United States 2012. The Journal of Pain: 16(8):769-780, as cited in the National Pain Strategy: A Comprehensive Population Health-Level Strategy for Pain, United States Department of Health and Human Services, iprcc.nih.gov/National_Pain_Strategy/NPS_Main.htm. —chronic pain has not always been well understood. The medical profession used to believe that pain was always a manifestation of an underlying injury or disease. Doctors focused on treating the cause of the pain, with the belief that the chronic pain would disappear once the injury or disease was cured.
If no underlying cause could be found, the patient was told that very few treatments are available, or worse—that “the pain must be in your head.” Some doctors still practice in this manner, having no appreciation for the unique problem of chronic pain, newer theories about chronic pain, and the many factors that influence a chronic pain problem.
Fortunately, efforts to focus public attention on the problem of chronic pain care have been encouraging in recent years. A National Pain Strategy, drawing on the efforts of patient advocates, scientists, and governmental experts, was released in 2016 by the Department of Health and Human Services. The strategy proposed improved access to quality care and better tracking to determine which therapies are most effective.
How Pain Affects the Brain
Chronic pain leads to brain changes, anxiety, and depression.
The medical community is starting to understand that if pain is no longer a function of a healthy nervous system, chronic pain itself becomes the problem.
Advanced neuroimaging has shown that chronic pain—unlike acute, or short-term pain—can cause structural changes in the brain that add to the risk of cognitive problems as well as anxiety and depression.3Borsook D. A Future Without Chronic Pain: Neuroscience and Clinical Research. Cerebrum. 2012 May-June; 2012:7.
In addition, studies of brain physiology have shown the central nervous system can change, based on a person's experiences. Medications and health conditions such as anxiety and depression can play a role in these changes.4Henry DE, Chiodo AE, Yang W. Central nervous system reorganization in a variety of chronic pain states: a review. PM R. 2011;3:11161125.
Pain May Not Be Recognized
While a broken leg can be confirmed by an X-ray, and an infection can be confirmed by a blood test to measure white blood cell count, there is no medical test to measure chronic pain levels. Thus, many people with chronic pain go from one doctor to the next searching for explanations. This process can lead to unnecessary evaluations and treatments.
See Getting an Accurate Back Pain Diagnosis
A further complication in getting care is that everyone experiences and expresses pain differently. Two people with the same injury will feel and show their pain in unique ways depending on a number of factors such as:
- The circumstances in which the pain occurs
- Thoughts about the chronic pain, such as “this is nothing serious” versus “this pain could kill me”
- Emotions associated with the chronic pain, such as depression and anxiety versus hopefulness and optimism
- Cultural influences leading a person to be more stoic or more dramatic in showing pain to others
Contrary to what some people believe, all pain is real. This may seem obvious, but people with chronic pain are sometimes treated as if their chronic pain is either imaginary or exaggerated. In some cases, they feel they have to prove their chronic pain to their friends, family, and doctors. Some patients are told by their doctor that there is no reason for the chronic pain and therefore “it cannot be that bad.”
- 1 Johannes C, et al. The Prevalence of Chronic Pain in United States Adults: Results of an Internet-Based Survey. J Pain. 2010 November; 11(11): 1230–1239, as cited in the National Pain Strategy: A Comprehensive Population Health-Level Strategy for Pain, United States Department of Health and Human Services, iprcc.nih.gov/National_Pain_Strategy/NPS_Main.htm.
- 2 Nahin, R. 2015 Estimates of Pain Prevalence and Severity in Adults: United States 2012. The Journal of Pain: 16(8):769-780, as cited in the National Pain Strategy: A Comprehensive Population Health-Level Strategy for Pain, United States Department of Health and Human Services, iprcc.nih.gov/National_Pain_Strategy/NPS_Main.htm.
- 3 Borsook D. A Future Without Chronic Pain: Neuroscience and Clinical Research. Cerebrum. 2012 May-June; 2012:7.
- 4 Henry DE, Chiodo AE, Yang W. Central nervous system reorganization in a variety of chronic pain states: a review. PM R. 2011;3:11161125.