Getting an accurate diagnosis for a cervical herniated disc can help to understand the underlying pain mechanisms involved, such as which nerve root might be compressed. An accurate diagnosis also plays an important role in getting the most effective treatment.
In This Article:
Cervical Herniated Disc Causes
Age-related degeneration is a common cause of cervical herniation.
Common causes of cervical herniated disc include:
- Disc degeneration over time. As a disc ages, it naturally loses hydration and becomes less flexible and durable. Cracks and tears are more likely to develop in a disc that has a lower water content.
- Trauma. A direct impact on the spine can cause a disc to tear or herniate.
Other less common causes of herniated discs are possible, such as connective tissue disorders or other abnormalities in the spine.
Cervical Herniated Disc Diagnosis
An MRI scan is a useful diagnostic tool to diagnose cervical herniated disc.
Getting an accurate diagnosis for a cervical herniated disc typically involves a 3-step process:
- Patient history. The patient’s medical history is reviewed, including any chronic conditions, past injuries, or history of back or neck pain. Information about the current symptoms is also gathered.
- Physical examination. The neck may be palpated (felt) for any areas of swelling, tenderness, or pain. The doctor also checks the neck’s range of motion, as well as for any signs of neurological deficits in the arms, such as issues with reflexes, numbness, and/or weakness.
- Imaging study. An imaging study can show whether a disc has started to flatten out or move beyond its normal location. A magnetic resonance imaging (MRI) scan is the preferred method for viewing a herniated disc due to its high-quality view of soft tissues. If an MRI is not an option, a CT or CT myelogram may also be considered.
In many cases, enough information can be gathered during the patient history and physical examination to begin treatment, so an imaging study is not always requested right away. However, to diagnose a cervical herniated disc as the cause of pain typically requires comparing the patient history, physical exam, imaging study, and an x-ray guided, contrast-enhanced diagnostic injection.
Read more about Diagnosing Neck Pain
Contained Vs. Uncontained Herniated Disc
When viewed during an imaging study, a cervical herniated disc can be classified in two general categories:
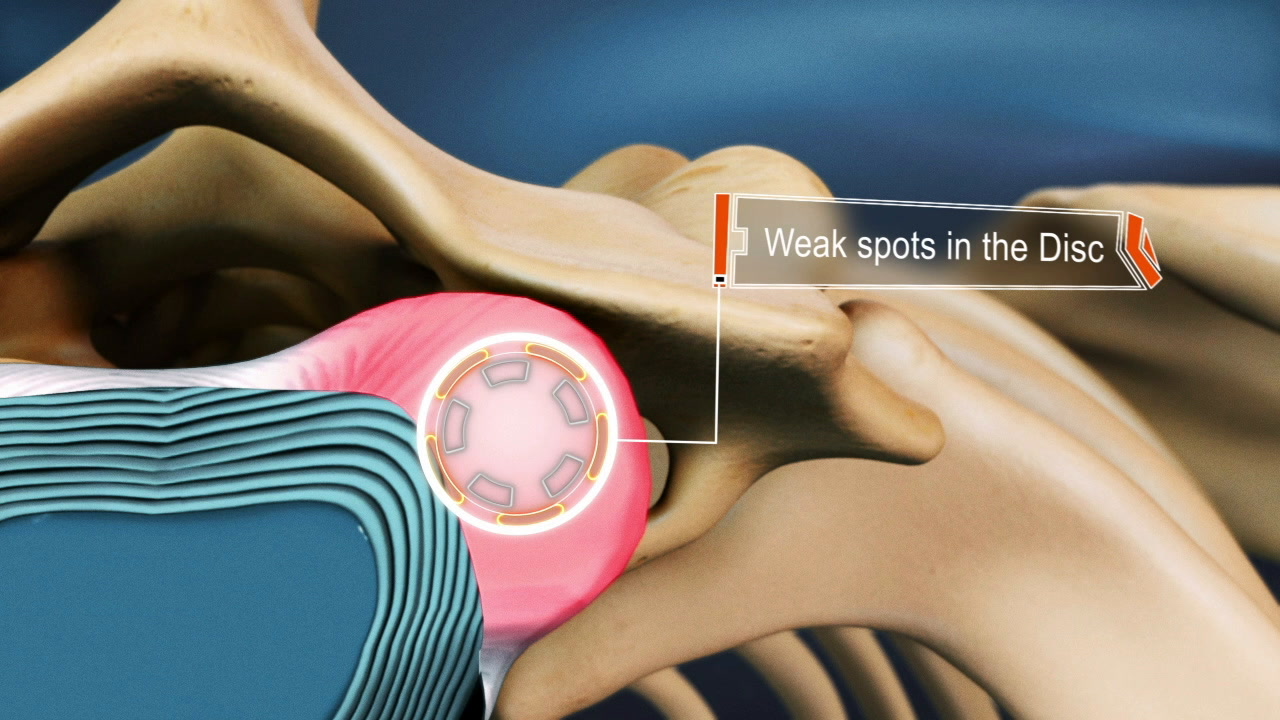
- Contained. A contained herniated disc involves the nucleus pulposus leaking into partial tears in the annulus fibrosus but not beyond the disc’s outermost layer. The disc may deform outward and still cause pain, such as by pressing against a nerve root or the spinal cord, but the nucleus pulposus and its inflammatory proteins remain inside the disc. A contained herniated disc is known as disc protrusion.
- Uncontained. An uncontained herniated disc occurs when the nucleus pulposus starts to leak through a complete tear in the annulus fibrosus and exits the disc’s outermost layer. Inflammatory proteins may leak onto a nerve root, the spinal cord, or other nearby tissues. An uncontained herniated disc is also known as disc extrusion. If some of the disc completely separates from the rest of the disc, it is called disc sequestration.
Watch Video: Can Herniated Discs Heal on Their Own?
A contained herniated disc may eventually become uncontained over time, but not always. It should also be noted that pain from either contained or uncontained discs can range from severe to no symptoms at all.