The experience of back pain can be complex. Many back problems are difficult to diagnose and typically involve a wide variety of treatment options with various risks and benefits. Also, there are many myths and misconceptions about back pain, and some misunderstandings can lead to harmful coping strategies and prolonged recovery times.
In the belief that high-quality education on the variety of back problems can be an effective adjunct to proper treatment, this article puts to rest a number of the more common misconceptions about back problems—the general myths, myths about diagnoses and causes of back pain, and myths about treatment options for back problems.
In This Article:
- The Myths and Reality of Back Pain and Back Problems
- Myths about Causes of Back Pain and Back Problems
Myth: Back Pain Can Result in Paralysis
Truth: The spinal structures are typically strong and resilient and have excellent healing capabilities when treated appropriately. The common causes of back pain are often problems within the bony tissues, like a spinal vertebral fracture, or damage to the soft tissues, such as muscles, ligaments, nerve roots, or spinal discs.
For paralysis to occur, the sensitive inner structures of the spine, such as the spinal cord or cauda equina (a group of spinal nerves that descend from the spinal cord) must be affected to a degree that the nervous transmission of sensory and motor signals are decreased or lost. This occurrence is rare because:
- The spinal cord and cauda equina are well protected within the spinal canal by strong ligamentous, bony, and muscular tissues.
- Even if the spinal cord and/or the cauda equina are affected, prompt treatment can help relieve and decompress these tissues, preventing long-term complications, such as paralysis.
Back pain paralysis symptoms often indicate cauda equina syndrome, a rare condition where the cauda equina nerves are compressed. Typical symptoms include numbness in the genital and groin regions and intolerable leg pain. If treated promptly, within 24 to 48 hours, the symptoms can be relieved and permanent nerve damage can be avoided.1Kim K-H, Kim DH. Diagnosis and Treatment of Spinal Pain. In: Minimally Invasive Percutaneous Spinal Techniques. Elsevier; 2010:1-28.,2Fairbank J, Mallen C. Cauda equina syndrome: implications for primary care. Br J Gen Pract. 2014;64(619):67–68. doi:10.3399/bjgp14X676988,3Petr O, Glodny B, Brawanski K, et al. Immediate Versus Delayed Surgical Treatment of Lumbar Disc Herniation for Acute Motor Deficits. SPINE. 2019;44(7):454-463. doi:10.1097/brs.0000000000002295 Cauda equina syndrome usually occurs due to spinal cord compression from a lumbar herniated disc and affects 1 in 30,000 to 100,000 people per year.4Rider LS, Marra EM. Cauda Equina And Conus Medullaris Syndromes. [Updated 2020 Aug 10]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK537200/
Read more about Cauda Equina Syndrome Symptoms
Myth: Back Pain Is Always Caused by an Injury
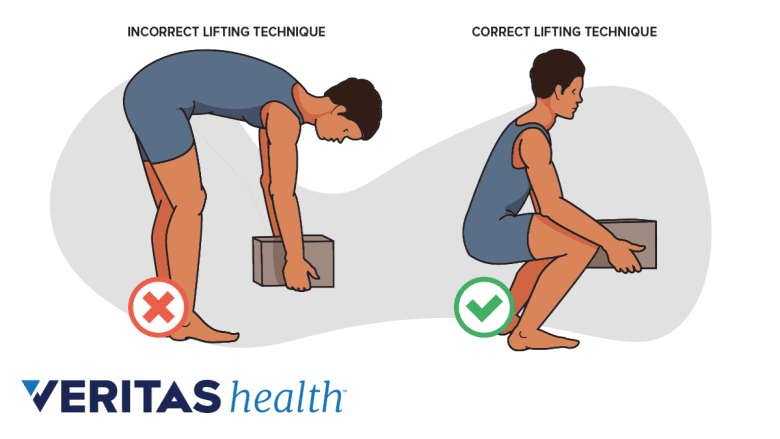
Using incorrect lifting techniques may increase the risk of back injury, leading to lower back pain.
Truth: The vast majority of back problems develop over time and may be due to wear-and-tear from repetitive trauma or unsupported posture. In contrast, a back injury is usually described as a one-time event and may occur from a motor vehicle collision, incorrect lifting technique, or a fall from the stairs.
The risk of developing back pain due to an injury is usually higher in individuals who have poorly conditioned tissues or who have an underlying condition, such as a bulging disc, which may suddenly herniate, causing the symptoms to exacerbate.
Any new development of back pain after a trauma, such as a sports injury or a fall, should be evaluated.
Myth: Severe Back Pain Indicates a Serious Problem
A pulled back muscle causes acute pain but is generally a self-limiting issue.
Truth: When the lower back hurts, the symptoms can range from mild to severe. These symptoms may indicate a minor, treatable, and/or self-limiting problem, such as a pulled back muscle or an overstretched ligament, or a more debilitating condition that affects the spinal nerves and/or discs.
The nature and severity of symptoms usually differ from one person to the other. While a pulled muscle in the lower back can send intense flare-ups of pain, causing people to end up in the emergency room, a severely herniated disc may be in close proximity to a spinal nerve, and yet produce no symptoms.
See Understanding Different Types of Back Pain
Myth: Back Pain Is Not Related to Genetics
Genetics may play a role in certain low back conditions.
Truth: Just like the color of hair or eyes, research suggests that specific changes in the lower back tissues, including alterations in the biochemical, metabolic, and functional capabilities may be related to genetics. These changes are mostly seen as5Williams FM, Bansal AT, van Meurs JB, et al. Novel genetic variants associated with lumbar disc degeneration in northern Europeans: a meta-analysis of 4600 subjects. Ann Rheum Dis. 2013;72(7):1141-1148. doi:10.1136/annrheumdis-2012-201551:
- Dehydration of discs
- Loss of disc height
- Growth of osteophytes from the vertebrae and/or spinal facet joints
These changes are usually diagnosed as lumbar degenerative disc disease or osteoarthritis of the spine and may be inherited in up to 80% of people with these conditions.5Williams FM, Bansal AT, van Meurs JB, et al. Novel genetic variants associated with lumbar disc degeneration in northern Europeans: a meta-analysis of 4600 subjects. Ann Rheum Dis. 2013;72(7):1141-1148. doi:10.1136/annrheumdis-2012-201551
Myth: If No Specific Back Problem Is Found, the Pain Must Be Psychological
The complex anatomical structures in the back can make it difficult to pinpoint the exact source of pain.
Truth: Due to the spine’s complex structure and delicate tissues, many cases of back pain may not have a specific structural diagnosis or simple treatment. The pain, however, is still real.
Typically, there is no single test to detect the underlying cause of back pain, and doctors may use a combination of clinical and medical imaging tests to determine the lower back problem. Masquerading symptoms, such as referred pain from piriformis syndrome or sacroiliac joint dysfunction, can make the diagnosis more challenging.
For persistent or concerning back pain, it is advisable to consult a qualified spine specialist to rule out serious problems, such as an underlying tumor or infection.
- 1 Kim K-H, Kim DH. Diagnosis and Treatment of Spinal Pain. In: Minimally Invasive Percutaneous Spinal Techniques. Elsevier; 2010:1-28.
- 2 Fairbank J, Mallen C. Cauda equina syndrome: implications for primary care. Br J Gen Pract. 2014;64(619):67–68. doi:10.3399/bjgp14X676988
- 3 Petr O, Glodny B, Brawanski K, et al. Immediate Versus Delayed Surgical Treatment of Lumbar Disc Herniation for Acute Motor Deficits. SPINE. 2019;44(7):454-463. doi:10.1097/brs.0000000000002295
- 4 Rider LS, Marra EM. Cauda Equina And Conus Medullaris Syndromes. [Updated 2020 Aug 10]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK537200/
- 5 Williams FM, Bansal AT, van Meurs JB, et al. Novel genetic variants associated with lumbar disc degeneration in northern Europeans: a meta-analysis of 4600 subjects. Ann Rheum Dis. 2013;72(7):1141-1148. doi:10.1136/annrheumdis-2012-201551