The spinal discs are designed to meet structural and dynamic needs of the spine. Discs are strong enough to manage multiple planes of motion. The disc has several functions, including serving as an integral part of the joint at each spinal motion segment.
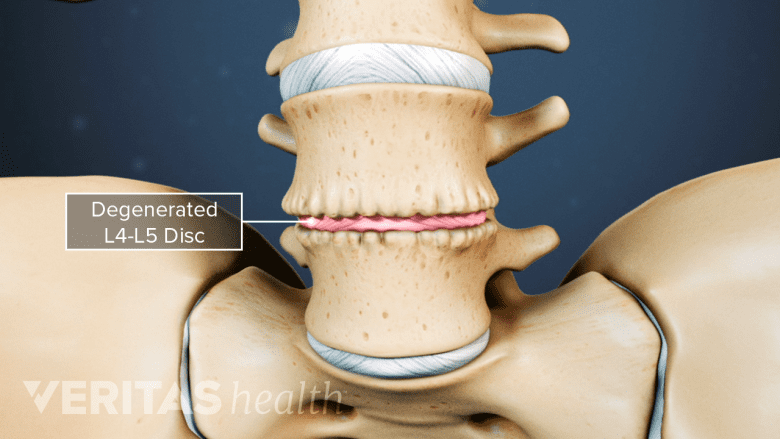
Over time, spinal discs tend to undergo complex structural, mechanical, and chemical changes and may become a source of pain. Even slight changes of disc nutrition and motion may cause a healthy, pristine disc to begin degenerating.
Aging may make the spinal disc more rigid and flat. As the structure changes, the disc becomes more susceptible to becoming a source of pain. Most people over 60 years old will have degenerative changes in the discs, but only a very small percent of people will experience pain. This article explains the process of disc degeneration.
In This Article:
Spinal Disc Anatomy and Function
A spinal disc is made of 2 layers: annulus fibrosis and nucleus pulposus.
Each spinal disc is one part of each of the motion segments that run along the length of the spinal column. The discs act as shock absorbers between the bony vertebral bodies; the flexibility of the discs allows the spine to resist multiple planes of motion created by various types of forces.
The intervertebral disc is comprised of a series of fibrous bands that form a tough outer layer and soft material with toothpaste consistency that forms a soft inner layer.
Annulus fibrosus
The disc’s outer layer is called the annulus fibrosus, named for the fibrous tissue that compose the layer. The fibers and water content of the annulus fibrosus exist in gradients. From the outer edge moving inwards, collagen type I fiber content decreases while protein and water content increase.1Eyre DR, Muir H. Types I and II collagens in intervertebral disc. Interchanging radial distributions in annulus fibrosus. Biochem J. 1976;157(1):267-270. doi:10.1042/bj1570267,2Urban J (1996). Disc biochemistry in relation to function. In: Wiesel SW, Weinstein JN, Herkowitz HN, Dvorak J, Bell G (eds) The lumbar spine. Saunders, Philadelphia, pp 271–280
Nucleus pulposus
The inner material contained in the disc is called the nucleus pulposus, named for the pulp-like or gel-like soft consistency of this layer.
Blood supply to the spinal disc
Blood vessels that supply nutrients to the disc lie in the endplates above and below it, rather than penetrating the disc itself.3Chen S, Fu P, Wu H, Pei M. Meniscus, articular cartilage and nucleus pulposus: a comparative review of cartilage-like tissues in anatomy, development and function. Cell Tissue Res. 2017;370(1):53-70. doi:10.1007/s00441-017-2613-0 Low blood supply limits nutrient delivery and slows the immune system response, particularly to tissues and cells damaged by age or injury.
Nerve endings in the spinal disc
In a healthy disc structure, nerves to the disc space only penetrate into the very outer edge of the annulus fibrosus.
If a tear in the annulus fibrosus reaches the outer edge, the nerves there can become sensitized and cause significant spine pain. With continued degradation, the nerve fibers on the periphery of the disc will actually grow further into the disc space. The growth of nerves may be associated with pain from a degenerating disc.4García-Cosamalón J, del Valle ME, Calavia MG, et al. Intervertebral disc, sensory nerves and neurotrophins: who is who in discogenic pain?. J Anat. 2010;217(1):1-15. doi:10.1111/j.1469-7580.2010.01227.x
If the nucleus pulposus, which contains a great deal of inflammatory proteins, leaks out of the disc and touches a nerve root, that nerve root can become inflamed and cause pain that radiates down a leg (sciatica or lumbar radiculopathy) or down an arm (cervical radiculopathy).
Degenerative Changes in the Spinal Discs
Degenerative disc disease occurs due to age-related wear-and-tear of a disc.
With age, the ability of the disc to tolerate a full range of motion decreases.5Stemper BD, Board D, Yoganandan N, Wolfla CE. Biomechanical properties of human thoracic spine disc segments. J Craniovertebr Junction Spine. 2010;1(1):18-22. doi:10.4103/0974-8237.65477 The cells and tissues of the disc can change in a progressive manner, contributing to the overall decrease in mechanical strength.
Discs degenerate in several ways over time.6Iatridis JC, MacLean JJ, O'Brien M, Stokes IA. Measurements of proteoglycan and water content distribution in human lumbar intervertebral discs. Spine (Phila Pa 1976). 2007;32(14):1493-1497. doi:10.1097/BRS.0b013e318067dd3f,7Cloyd JM, Elliott DM. Elastin content correlates with human disc degeneration in the anulus fibrosus and nucleus pulposus. Spine (Phila Pa 1976). 2007;32(17):1826-1831. doi:10.1097/BRS.0b013e3181132a9d,8Raj PP. Intervertebral disc: anatomy-physiology-pathophysiology-treatment. Pain Pract. 2008;8(1):18-44. doi:10.1111/j.1533-2500.2007.00171.x
- Elastin fiber content increases, especially in the inner edge of the annulus fibrosus.
- Osmotic pressure, needed to maintain high water content in the nucleus, decreases.
- Water content decreases, from 80% at birth to as low as 66% in the sixth decade of life.
- Disc height decreases.
High water content gives the disc its spongy quality and shock-absorbing ability. With age and degeneration, the disc gradually loses its ability to absorb shock and its flexibility.
Other characteristics of an aging, dehydrating disc include9Vo NV, Hartman RA, Patil PR, et al. Molecular mechanisms of biological aging in intervertebral discs. J Orthop Res. 2016;34(8):1289-1306. doi:10.1002/jor.23195,10Hormel SE, Eyre DR. Collagen in the ageing human intervertebral disc: an increase in covalently bound fluorophores and chromophores. Biochim Biophys Acta. 1991;1078(2):243-250. doi:10.1016/0167-4838(91)90565-h:
- Yellowing of the nucleus pulposus
- Small fractures in the adjacent bones
- Thickening of the adjacent bones
- Thinning of the cartilaginous endplates
- Fewer blood vessels in the endplates
As the blood vessels that serve the disc decrease in number, build-up of cellular waste grows. The build-up in the disc can decrease pH to as low as 6.3, making the interior of the disc more acidic and risking further cellular damage with age and with stress.11Bibby SR, Jones DA, Ripley RM, Urban JP. Metabolism of the intervertebral disc: effects of low levels of oxygen, glucose, and pH on rates of energy metabolism of bovine nucleus pulposus cells. Spine (Phila Pa 1976). 2005;30(5):487-496. doi:10.1097/01.brs.0000154619.38122.47
The degenerating disc can cause structural changes nearby, such as the narrowing of a nerve pathway which causes spinal stenosis and may result in radicular pain.
Degenerative Disc Disease Pain
Inflammatory proteins that leak from the disc's core trigger inflammation and pain.
While disc degeneration does not necessarily cause pain, research has shown that disc degeneration is strongly associated with cases of low back pain.12Kos N, Gradisnik L, Velnar T. A Brief Review of the Degenerative Intervertebral Disc Disease. Med Arch. 2019;73(6):421-424. doi:10.5455/medarh.2019.73.421-424 Pain may be debilitating in nature and restrict mobility.
Disc pain may be caused by several factors acting simultaneously, usually involving nerves that penetrate deep into the disc’s outer edge or involving the instability of the disc after an injury.
- Inflammation. The proteins in the disc interior cause inflammation if they come into contact with nearby muscles, joints, and nerve roots. Inflammation can cause pain, increased muscle tension, muscle spasms, and tenderness around the affected disc, as well as sharp, shooting pains in the leg or in the arm if a nerve root is affected (sciatica, or cervical radiculopathy respectively.)
- Disc space collapse. Decreasing disc height and water content place undue strain on the joints and muscles that support the vertebrae. In some cases, a collapsed disc space can cause a nerve root to become pinched or irritated, leading to pain in the arm or leg.
- Excessive micro-motions. Decreased cushioning and support from the disc may lead to relative increase in motion between two vertebrae. This excess motion typically causes muscle spasm and pain, may irritate the joints and nerve roots, and can result in formation of bone spurs.
Pain may range from mild to severe, and may become worse with certain positions, such as prolonged standing or sitting, or with certain movements, such as twisting or bending the spine. The process of how a disc degenerates has been studied and is thought to follow a typical pattern that occurs over a long period of time- several years or decades.
- 1 Eyre DR, Muir H. Types I and II collagens in intervertebral disc. Interchanging radial distributions in annulus fibrosus. Biochem J. 1976;157(1):267-270. doi:10.1042/bj1570267
- 2 Urban J (1996). Disc biochemistry in relation to function. In: Wiesel SW, Weinstein JN, Herkowitz HN, Dvorak J, Bell G (eds) The lumbar spine. Saunders, Philadelphia, pp 271–280
- 3 Chen S, Fu P, Wu H, Pei M. Meniscus, articular cartilage and nucleus pulposus: a comparative review of cartilage-like tissues in anatomy, development and function. Cell Tissue Res. 2017;370(1):53-70. doi:10.1007/s00441-017-2613-0
- 4 García-Cosamalón J, del Valle ME, Calavia MG, et al. Intervertebral disc, sensory nerves and neurotrophins: who is who in discogenic pain?. J Anat. 2010;217(1):1-15. doi:10.1111/j.1469-7580.2010.01227.x
- 5 Stemper BD, Board D, Yoganandan N, Wolfla CE. Biomechanical properties of human thoracic spine disc segments. J Craniovertebr Junction Spine. 2010;1(1):18-22. doi:10.4103/0974-8237.65477
- 6 Iatridis JC, MacLean JJ, O'Brien M, Stokes IA. Measurements of proteoglycan and water content distribution in human lumbar intervertebral discs. Spine (Phila Pa 1976). 2007;32(14):1493-1497. doi:10.1097/BRS.0b013e318067dd3f
- 7 Cloyd JM, Elliott DM. Elastin content correlates with human disc degeneration in the anulus fibrosus and nucleus pulposus. Spine (Phila Pa 1976). 2007;32(17):1826-1831. doi:10.1097/BRS.0b013e3181132a9d
- 8 Raj PP. Intervertebral disc: anatomy-physiology-pathophysiology-treatment. Pain Pract. 2008;8(1):18-44. doi:10.1111/j.1533-2500.2007.00171.x
- 9 Vo NV, Hartman RA, Patil PR, et al. Molecular mechanisms of biological aging in intervertebral discs. J Orthop Res. 2016;34(8):1289-1306. doi:10.1002/jor.23195
- 10 Hormel SE, Eyre DR. Collagen in the ageing human intervertebral disc: an increase in covalently bound fluorophores and chromophores. Biochim Biophys Acta. 1991;1078(2):243-250. doi:10.1016/0167-4838(91)90565-h
- 11 Bibby SR, Jones DA, Ripley RM, Urban JP. Metabolism of the intervertebral disc: effects of low levels of oxygen, glucose, and pH on rates of energy metabolism of bovine nucleus pulposus cells. Spine (Phila Pa 1976). 2005;30(5):487-496. doi:10.1097/01.brs.0000154619.38122.47
- 12 Kos N, Gradisnik L, Velnar T. A Brief Review of the Degenerative Intervertebral Disc Disease. Med Arch. 2019;73(6):421-424. doi:10.5455/medarh.2019.73.421-424