Isthmic spondylolisthesis is a condition where a spinal vertebra slips forward on the one below it due to a structural defect in the small piece of bone, the pars interarticularis, which connects the two vertebrae on the back of the spine.1Burton MR, Dowling TJ, Mesfin FB. Isthmic Spondylolisthesis. [Updated 2022 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441846/
Isthmic spondylolisthesis can occur in the neck, upper back, or lower back, but primarily occurs in the lower back and typically doesn’t cause any symptoms. About 25% of people who have isthmic spondylolisthesis may develop symptoms, and the most common symptoms include chronic back pain with or without leg pain (sciatica).1Burton MR, Dowling TJ, Mesfin FB. Isthmic Spondylolisthesis. [Updated 2022 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441846/,2Bhalla A, Bono CM. Isthmic lumbar spondylolisthesis. Neurosurgery Clinics of North America. 2019;30(3):283-290. doi:10.1016/j.nec.2019.02.001
In This Article:
Isthmic vs Degenerative Spondylolisthesis: Understanding the Key Difference
It is important to note that a similar type of vertebral slip can also occur due to degenerative spinal changes from aging, in which case the condition is called degenerative spondylolisthesis.
While the symptoms of both these conditions may overlap, the underlying causes and risk factors are distinct.
Understanding The Mechanism and Progression of Isthmic Spondylolisthesis
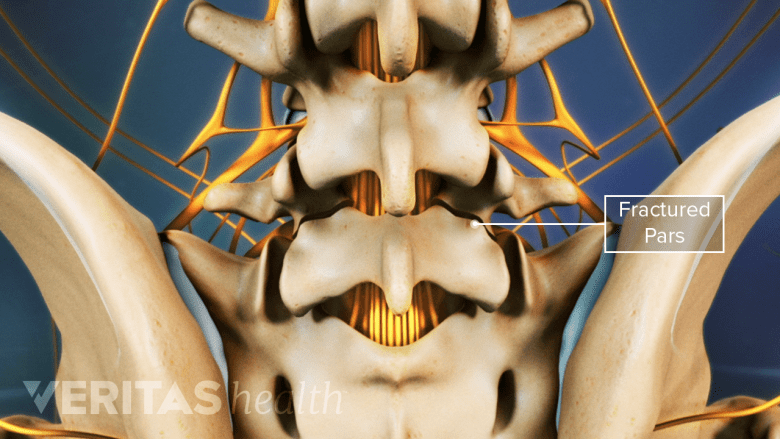
The mechanism of isthmic spondylolisthesis revolves around the integrity of a small bony bridge in the back of the spine, called the pars interarticularis. This bridge is a thin piece of bone, which connects the upper and lower facet joints on the back of each vertebra.1Burton MR, Dowling TJ, Mesfin FB. Isthmic Spondylolisthesis. [Updated 2022 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441846/
1. Fracture of the pars and forward displacement of the vertebra
A broken pars interarticularis bone can compromise spinal stability.
Research shows that the pars is subjected to the greatest force compared to any other structure in the lumbar spine, making it susceptible to stress fractures. In susceptible individuals, the pars may fracture, heal, and fracture again—repeatedly.1Burton MR, Dowling TJ, Mesfin FB. Isthmic Spondylolisthesis. [Updated 2022 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441846/
In most cases, pars fractures are believed to be the result of repetitive motion. Other causes include trauma, or a congenital defect, weakening the structure of the pars bone.1Burton MR, Dowling TJ, Mesfin FB. Isthmic Spondylolisthesis. [Updated 2022 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441846/
The fracture of the pars interarticularis is known as a spondylolysis.3Pereira Duarte M, Camino Willhuber GO. Pars Interarticularis Injury. [Updated 2023 Feb 5]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK545191/
Watch Lumbar Spondylolysis Video
Over time, spondylolysis can progress, leading to the slip of one vertebra over the other—called spondylolisthesis. This slip always occurs in a forward direction and disrupts the normal alignment of the spine, causing instability and abnormal movement between the affected vertebrae.
The most commonly affected spinal segment is the L5-S1 spinal motion segment in the lower back.1Burton MR, Dowling TJ, Mesfin FB. Isthmic Spondylolisthesis. [Updated 2022 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441846/
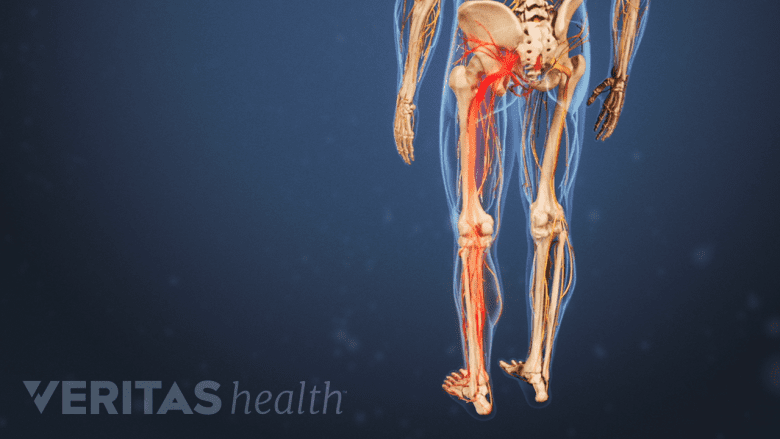
2. Nerve compression and pain
Spondylolisthesis can cause compression of spinal nerves, resulting in sciatica.
The degree of vertebral slippage can worsen with time, causing impingement or compression of the nearby spinal nerve roots and/or the spinal cord. This process can cause a range of symptoms, including back pain, radiating leg pain (sciatica), numbness, tingling, and muscle weakness. The severity of symptoms varies depending on the degree of slip and the structures affected.
See Leg Pain and Numbness: What Might These Symptoms Mean?
The L5 nerve root exiting the L5-S1 spinal segment is most commonly affected by this condition.4Mesfin FB. Isthmic Spondylolisthesis. [Updated 2022 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441846/
Watch L5-S1 Isthmic Spondylolisthesis Animation
3. Degenerative changes and compensatory mechanisms
Overtime, isthmic spondylolisthesis can cause degenerative changes in the vertebrae and disc.
Isthmic spondylolisthesis can also lead to degenerative changes in the affected spinal segment. The slipped vertebra increases the stress within the affected segment, leading to abnormal motion between the vertebrae. This abnormal motion can accelerate wear and tear on the intervertebral discs, facet joints, and surrounding structures.4Mesfin FB. Isthmic Spondylolisthesis. [Updated 2022 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441846/
As a compensatory mechanism, the body may initiate the growth of abnormal bone, called bone spurs or osteophytes, further impacting the structural integrity of the spinal segment.4Mesfin FB. Isthmic Spondylolisthesis. [Updated 2022 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441846/
The Grades of Isthmic Spondylolisthesis: Classifying Severity and Implications
The severity of the slippage is usually measured after taking a side-view x-ray, and then graded on a scale of 1 to 5 (also called Meyerding’s classification). A measurement of the amount the upper vertebral body slips forward on the lower vertebral body is taken.5Tenny S, Gillis CC. Spondylolisthesis. [Updated 2023 May 22]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430767/
| Grade of Isthmic Spondylolisthesis | Measurement of Vertebral Slippage5Tenny S, Gillis CC. Spondylolisthesis. [Updated 2023 May 22]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430767/ |
|---|---|
| Grade 1 | <25% of the vertebral body has slipped forward |
| Grade 2 | 26% - 50% of the vertebral body has slipped forward |
| Grade 3 | 51% - 75% of the vertebral body has slipped forward |
| Grade 4 | 76% - 100% of the vertebral body has slipped forward |
| Grade 5 (Spondyloptosis) | >100% of the vertebral body has slipped forward |
Although very rare, the L5 vertebral body may slip off the sacrum and into the pelvis. This condition is called spondyloptosis and warrants surgical treatment.
Based on the type of fracture of the pars interarticularis, isthmic spondylolisthesis may be classified5Tenny S, Gillis CC. Spondylolisthesis. [Updated 2023 May 22]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430767/:
- Subtype A: Stress fractures of the pars
- Subtype B: Elongation of the pars without overt fracture
- Subtype C: Acute fracture of the pars
In general, children are at a higher risk of spondylolisthesis grade progression during puberty. Older patients with lower grades of spondylolistheses (grades 1 or 2) are less likely to progress to higher grades over time.5Tenny S, Gillis CC. Spondylolisthesis. [Updated 2023 May 22]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430767/
About 75% of all the diagnosed spondylolistheses cases are grade 1.5Tenny S, Gillis CC. Spondylolisthesis. [Updated 2023 May 22]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430767/
Isthmic Spondylolisthesis in Children and Teens
High-intensity sports are a risk factor for pars interarticularis fracture in kids.
In children and adolescents, isthmic spondylolisthesis may sometimes be attributed to a congenital defect in the pars interarticularis.6Mansfield JT, Wroten M. Pars Interarticularis Defect. [Updated 2022 Aug 21]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK538292/ Congenital isthmic spondylolisthesis occurs when the pars interarticularis is abnormally formed from birth.
Stress fractures of the pars interarticularis typically occurs in kids 4 to 6 years of age due to repetitive stress or trauma, often associated with activities that place a high demand on the spine, such as gymnastics, football, or weightlifting.6Mansfield JT, Wroten M. Pars Interarticularis Defect. [Updated 2022 Aug 21]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK538292/,7Studnicka K, Ampat G. Lumbosacral Spondylolisthesis. [Updated 2022 Sep 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK560679/
Isthmic Spondylolisthesis in Athletes
Sports like weightlifting can cause pars fractures in adults.
Isthmic spondylolisthesis in athletes typically occurs due to repetitive stress, high-impact activities, and certain sports-related movements that place significant strain on the lower back.8Mohile NV, Kuczmarski AS, Lee D, Warburton C, Rakoczy K, Butler AJ. Spondylolysis and isthmic spondylolisthesis: a guide to diagnosis and management. J Am Board Fam Med. 2022;35(6):1204-1216. doi:10.3122/jabfm.2022.220130R1
Gymnastics, weightlifting, football, and other sports involving repetitive spinal hyperextension (bending backwards) or rotation are commonly associated with this condition.8Mohile NV, Kuczmarski AS, Lee D, Warburton C, Rakoczy K, Butler AJ. Spondylolysis and isthmic spondylolisthesis: a guide to diagnosis and management. J Am Board Fam Med. 2022;35(6):1204-1216. doi:10.3122/jabfm.2022.220130R1
When Isthmic Spondylolisthesis Is Serious
If isthmic spondylolisthesis symptoms occur suddenly after a major trauma or injury, such as a fall or car accident, medical attention should be sought immediately. These incidents can cause fractures or worsen existing spondylolisthesis, leading to spinal instability and potential neurological complications.
Additionally, recognizing the red flag symptoms and signs of isthmic spondylolisthesis is crucial to ensure timely medical attention and appropriate management.
Isthmic spondylolisthesis may require urgent care or become a medical emergency if the following signs or symptoms occur:
Progressive pain and weakness
Pain that gets worse over time or affects both legs must be evaluated by a physician.
Persistent and/or progressive pain in the lower back that interferes with daily activities or worsens over time warrants immediate medical attention. The pain may radiate into the buttocks, thighs, or legs, and may be accompanied by numbness, tingling, or muscle weakness.
Similarly, the progression of neurological symptoms, such as muscle weakness, and/or loss of sensation, should be evaluated by a physician on an urgent basis.
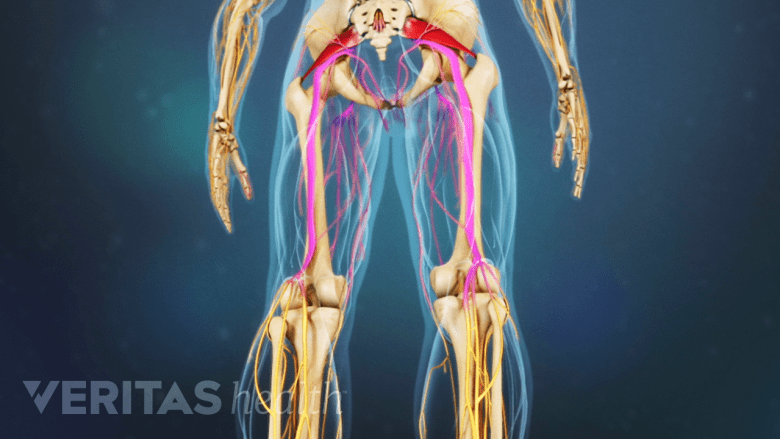
Altered bowel or bladder function
Damage to the cauda equina nerves can cause loss of motor function in the lower body.
Changes in bowel or bladder function, such as difficulty controlling or emptying the bladder, bowel incontinence, or experiencing numbness in the genital area, is a medical emergency. These symptoms indicate cauda equina syndrome, a rare but serious condition that requires urgent surgical intervention.
Significant loss of function or mobility
Inability to perform foot movements must be evaluated by a doctor.
Difficulty walking, balancing, or performing basic movements may indicate a more advanced stage of the condition that requires medical intervention. Prompt evaluation by a healthcare professional, accurate diagnosis, and tailored treatment can help control pain, prevent further complications, and improve overall quality of life for individuals with isthmic spondylolisthesis.
- 1 Burton MR, Dowling TJ, Mesfin FB. Isthmic Spondylolisthesis. [Updated 2022 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441846/
- 2 Bhalla A, Bono CM. Isthmic lumbar spondylolisthesis. Neurosurgery Clinics of North America. 2019;30(3):283-290. doi:10.1016/j.nec.2019.02.001
- 3 Pereira Duarte M, Camino Willhuber GO. Pars Interarticularis Injury. [Updated 2023 Feb 5]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK545191/
- 4 Mesfin FB. Isthmic Spondylolisthesis. [Updated 2022 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441846/
- 5 Tenny S, Gillis CC. Spondylolisthesis. [Updated 2023 May 22]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430767/
- 6 Mansfield JT, Wroten M. Pars Interarticularis Defect. [Updated 2022 Aug 21]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK538292/
- 7 Studnicka K, Ampat G. Lumbosacral Spondylolisthesis. [Updated 2022 Sep 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK560679/
- 8 Mohile NV, Kuczmarski AS, Lee D, Warburton C, Rakoczy K, Butler AJ. Spondylolysis and isthmic spondylolisthesis: a guide to diagnosis and management. J Am Board Fam Med. 2022;35(6):1204-1216. doi:10.3122/jabfm.2022.220130R1