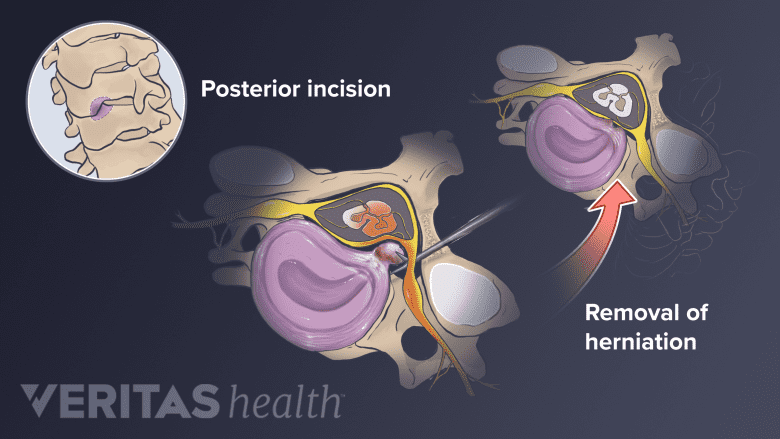
Some spine surgeons may prefer the posterior approach (from the back of the neck) for a cervical discectomy. This approach is often considered for large soft disc herniations that are lateral to (to the side of) the spinal cord.
Posterior Discectomy Advantages and Disadvantages
- The principal advantage of the posterior approach is that a spine fusion does not need to be done after removing the disc.
- The principal disadvantage is that the disc space cannot be jacked open with a bone graft to give more space to the nerve root as it exits the spine. Also, since the posterior approach leaves most of the disc in place, there is a small chance (3% to 5%) that a disc herniation may recur in the future.
What Occurs During Posterior Cervical Decompression?
The general procedure for the posterior cervical decompression (microdiscectomy) surgery includes the:
- Surgical approach.
- A small incision is made in the midline of the back of the neck.
- The para-spinal muscles are elevated off the spinal level that is to be approached.
- Disc removal.
- An x-ray is done to confirm that the surgeon is at the correct level of the spine.
- A high-speed burr is used to remove some of the facet joint, and the nerve root is then identified under the facet joint.
- An operating microscope is then used for better visualization.
- The disc will be directly under the nerve root, which needs to be gently mobilized (moved to the side) to free up the disc herniation.
- There is usually a plexus (network) of veins over the disc that can obstruct visualization if they bleed.
Posterior Cervical Discectomy Risks and Complications
Possible risks and complications of a posterior approach for cervical discectomy include:
- Nerve root damage
- Spinal cord damage
- Dural leak
- Infection
- Bleeding
- Continued pain
- Recurrent disc herniation.
In general, however, complications are rare.
Posterior Versus Anterior Cervical Discectomy
The major advantage of approaching a cervical disc herniation through a posterior approach is that a fusion need not be performed. This preserves the normal motion of the cervical spine, and may provide for a shorter healing time.
Although avoiding a fusion may sound desirable, the posterior approach has many disadvantages.
- Because the spinal cord is in the way, visualization of the disc space is limited, and typically only a disc herniation that is lateral (off to the side of the spine) can be approached.
- Also, by not doing a fusion from the anterior, the disc space is not distracted and the associated collapse that happens with a disc herniation can continue and place pressure on the nerve in the foramen (where the nerve exits the spine).
- Lastly, since the disc is not removed completely, it can re-herniate in the future.
In general, most surgeons prefer approaching the cervical spine from the anterior when possible because it is:
- A more reliable and definitive procedure
- Generally less demanding technically than a posterior approach.