Serious health complications, such as foot ulcers and retinopathy (damaged blood vessels in the back of the eye), are commonly associated with diabetes. However, signs of diabetes disease progression have also been linked to chronic back pain,1Rinaldo L, McCutcheon BA, Gilder H, et al. Diabetes and Back Pain: Markers of Diabetes Disease Progression Are Associated With Chronic Back Pain. Clin Diabetes. 2017;35(3):126-131. doi:10.2337/cd16-0011 suggesting that uncontrolled diabetes is likely to play a role in the development of chronic back pain. Additional factors related to diabetes, such as clinical obesity, may also be linked to chronic back pain and related spinal disorders.
In This Article:
- Uncontrolled Diabetes Linked to Chronic Back Pain
- Types of Back Problems Linked to Diabetes
Diabetes Is a Risk Factor for Lower Back Pain
Diabetes-related blood sugar imbalances may increase the risk of low back pain.
Individuals with diabetes are 19% to 35% more likely to have lower back pain and 24% to 34% more likely to have neck pain than the general population.2Pozzobon D, Ferreira PH, Dario AB, et al. Is there an association between diabetes and neck and back pain? A systematic review with meta-analyses. PLoS One. 2019;14(2):e0212030. Published 2019 Feb 21. doi:10.1371/journal.pone.0212030,3Lima Florencio L, Lopez-de-Andres A, Hernández-Barrera V, et al. Is There an Association between Diabetes and Neck and Back Pain? Results of a Case-Control Study. J Clin Med. 2020;9(9):2867. Published 2020 Sep 4. doi:10.3390/jcm9092867 The noticeably higher risks of spinal pain may be the result of diabetes-related imbalances in blood sugar, insulin, and free radicals, which place unhealthy stress on spinal discs.
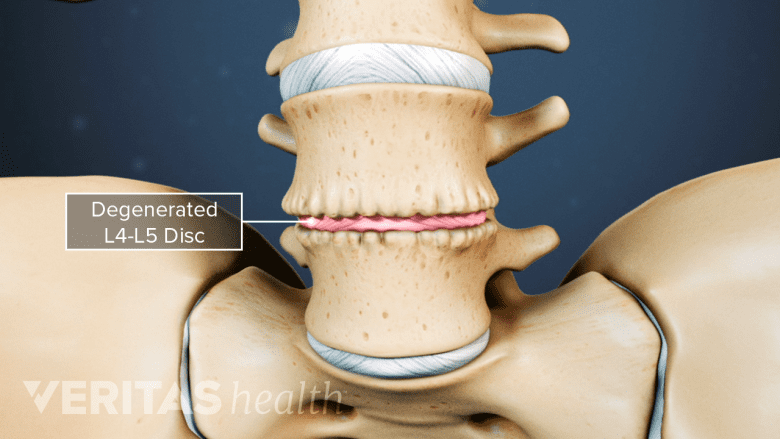
Several studies have connected spinal degeneration to uncontrolled diabetes and its markers,4Silberberg R, Adler JH, Meier-Ruge W. Effects of hyperinsulinism and of diabetes on proteoglycans of the intervertebral disc in weanling sand rats. Exp Cell Biol. 1986;54(3):121-127. doi:10.1159/000163449,5Robinson D, Mirovsky Y, Halperin N, Evron Z, Nevo Z. Changes in proteoglycans of intervertebral disc in diabetic patients. A possible cause of increased back pain. Spine (Phila Pa 1976). 1998;23(8):849-856. doi:10.1097/00007632-199804150-00001,6Cheng X, Ni B, Zhang Z, et al. Polyol pathway mediates enhanced degradation of extracellular matrix via p38 MAPK activation in intervertebral disc of diabetic rats. Connect Tissue Res. 2013;54(2):118-122. doi:10.3109/03008207.2012.754886,7Park EY, Park JB. Dose- and time-dependent effect of high glucose concentration on viability of notochordal cells and expression of matrix degrading and fibrotic enzymes. Int Orthop. 2013;37(6):1179-1186. doi:10.1007/s00264-013-1836-2,8Park EY, Park JB. High glucose-induced oxidative stress promotes autophagy through mitochondrial damage in rat notochordal cells. Int Orthop. 2013;37(12):2507-2514. doi:10.1007/s00264-013-2037-8,9Kong JG, Park JB, Lee D, Park EY. Effect of high glucose on stress-induced senescence of nucleus pulposus cells of adult rats. Asian Spine J. 2015;9(2):155-161. doi:10.4184/asj.2015.9.2.155,10Kong CG, Park JB, Kim MS, Park EY. High glucose accelerates autophagy in adult rat intervertebral disc cells. Asian Spine J. 2014;8(5):543-548. doi:10.4184/asj.2014.8.5.543 including:
- Hyperglycemia (high levels of sugar in the blood)
- Hyperinsulinemia (high levels of insulin in the blood)
- Oxidative stress (high levels of free radicals)
Free radicals refer to unstable atoms that damage cells and contribute to the aging of the body. Antioxidants, such as vitamin E, help to stabilize free radicals and prevent damage. If free radicals outnumber antioxidants, cells tend to become strained by the damage; this strain is referred to as oxidative stress.
Hyperglycemia
Diabetes is connected with high levels of sugar, namely glucose and sorbitol, which is a by-product of glucose. High blood sugar tends to change the extracellular matrix5Robinson D, Mirovsky Y, Halperin N, Evron Z, Nevo Z. Changes in proteoglycans of intervertebral disc in diabetic patients. A possible cause of increased back pain. Spine (Phila Pa 1976). 1998;23(8):849-856. doi:10.1097/00007632-199804150-00001 leading to increased rate of cell death, particularly for cells that form the inner ring of the intervertebral spinal disc. The inference here is that the natural aging of the disc accelerates due to these cellular changes.6Cheng X, Ni B, Zhang Z, et al. Polyol pathway mediates enhanced degradation of extracellular matrix via p38 MAPK activation in intervertebral disc of diabetic rats. Connect Tissue Res. 2013;54(2):118-122. doi:10.3109/03008207.2012.754886
See The "Degenerative Cascade" of a Degenerating Disc
Hyperinsulinemia
Persistent high insulin levels accelerate disc degeneration by altering its shape and function.
High levels of insulin in the blood, associated most closely with type 2 diabetes, leads to a slight change in the profile of proteoglycans (protein molecules that have attached carbohydrate chains). Excess insulin increases the amount of chondroitin sulfate, a type of proteoglycan, in the outer ring of the intervertebral discs of rats.3Lima Florencio L, Lopez-de-Andres A, Hernández-Barrera V, et al. Is There an Association between Diabetes and Neck and Back Pain? Results of a Case-Control Study. J Clin Med. 2020;9(9):2867. Published 2020 Sep 4. doi:10.3390/jcm9092867
Loss of this chondroitin sulfate lowers the water content of the disc, decreasing the disc’s flexibility and function. The proteoglycan profile in patients with diabetes has lower buoyant density and fewer sugar side chains compared to patients without diabetes.4Silberberg R, Adler JH, Meier-Ruge W. Effects of hyperinsulinism and of diabetes on proteoglycans of the intervertebral disc in weanling sand rats. Exp Cell Biol. 1986;54(3):121-127. doi:10.1159/000163449 Consistently elevated insulin levels alter the proteoglycans in several ways, leading to changes in the shape and function of the disc; the disc degenerates more quickly than in cases of controlled diabetes or cases without diabetes.
See What Is Degenerative Disc Disease?
Oxidative Stress
Additional studies of diabetic rats found that high glucose levels lead to oxidative stress, which occurs when the number of free radicals outweighs the number of antioxidants. Oxidative stress leads to damaged cells in the inner ring of the disc, contributing to accelerated aging of the disc. The effect of hyperglycemia worsened with higher glucose levels and with longer duration of hyperglycemia, demonstrating that diabetes may have a dose-dependent and time-dependent relationship with disc degeneration.7Park EY, Park JB. Dose- and time-dependent effect of high glucose concentration on viability of notochordal cells and expression of matrix degrading and fibrotic enzymes. Int Orthop. 2013;37(6):1179-1186. doi:10.1007/s00264-013-1836-2,8Park EY, Park JB. High glucose-induced oxidative stress promotes autophagy through mitochondrial damage in rat notochordal cells. Int Orthop. 2013;37(12):2507-2514. doi:10.1007/s00264-013-2037-8,9Kong JG, Park JB, Lee D, Park EY. Effect of high glucose on stress-induced senescence of nucleus pulposus cells of adult rats. Asian Spine J. 2015;9(2):155-161. doi:10.4184/asj.2015.9.2.155
Research suggests that hyperglycemia, hyperinsulinemia, and oxidative stress lead to significant changes, such as the composition of the proteoglycans in the spinal discs. These studies indicate that diabetes is likely to contribute to cellular changes and degeneration in the spine, beyond that of obesity or physical inactivity alone. More research needs to be done before a clear relationship between diabetes and disc degeneration can be truly established.
Read more about Causes of Degenerative Disc Disease Pain
Markers of Diabetes Correlate with Chronic Back Pain
In a study of tens of thousands of cases of diabetes, comparisons were made across 3 categories1Rinaldo L, McCutcheon BA, Gilder H, et al. Diabetes and Back Pain: Markers of Diabetes Disease Progression Are Associated With Chronic Back Pain. Clin Diabetes. 2017;35(3):126-131. doi:10.2337/cd16-0011:
- Diabetes with no chronic back pain
- Diabetes with chronic back pain
- Diabetes with surgical intervention for chronic back pain
Several variables were found to be associated with development of chronic back pain or having spinal surgery, such as neuropathy, retinopathy, insulin use, and higher body mass index (BMI), and more.1Rinaldo L, McCutcheon BA, Gilder H, et al. Diabetes and Back Pain: Markers of Diabetes Disease Progression Are Associated With Chronic Back Pain. Clin Diabetes. 2017;35(3):126-131. doi:10.2337/cd16-0011
The patients who underwent surgery for spinal disorders related to chronic back pain tended to have stronger indicators of diabetes progression than did the individuals who did not receive surgical treatment for their pain. An additional variable may be time; with every year that passes, the risk for developing chronic back pain increased in patients with diabetes.1Rinaldo L, McCutcheon BA, Gilder H, et al. Diabetes and Back Pain: Markers of Diabetes Disease Progression Are Associated With Chronic Back Pain. Clin Diabetes. 2017;35(3):126-131. doi:10.2337/cd16-0011
It is thought that the toll of uncontrolled diabetes on the body may contribute to specific spinal conditions and eventually a need for surgical treatment.
- 1 Rinaldo L, McCutcheon BA, Gilder H, et al. Diabetes and Back Pain: Markers of Diabetes Disease Progression Are Associated With Chronic Back Pain. Clin Diabetes. 2017;35(3):126-131. doi:10.2337/cd16-0011
- 2 Pozzobon D, Ferreira PH, Dario AB, et al. Is there an association between diabetes and neck and back pain? A systematic review with meta-analyses. PLoS One. 2019;14(2):e0212030. Published 2019 Feb 21. doi:10.1371/journal.pone.0212030
- 3 Lima Florencio L, Lopez-de-Andres A, Hernández-Barrera V, et al. Is There an Association between Diabetes and Neck and Back Pain? Results of a Case-Control Study. J Clin Med. 2020;9(9):2867. Published 2020 Sep 4. doi:10.3390/jcm9092867
- 4 Silberberg R, Adler JH, Meier-Ruge W. Effects of hyperinsulinism and of diabetes on proteoglycans of the intervertebral disc in weanling sand rats. Exp Cell Biol. 1986;54(3):121-127. doi:10.1159/000163449
- 5 Robinson D, Mirovsky Y, Halperin N, Evron Z, Nevo Z. Changes in proteoglycans of intervertebral disc in diabetic patients. A possible cause of increased back pain. Spine (Phila Pa 1976). 1998;23(8):849-856. doi:10.1097/00007632-199804150-00001
- 6 Cheng X, Ni B, Zhang Z, et al. Polyol pathway mediates enhanced degradation of extracellular matrix via p38 MAPK activation in intervertebral disc of diabetic rats. Connect Tissue Res. 2013;54(2):118-122. doi:10.3109/03008207.2012.754886
- 7 Park EY, Park JB. Dose- and time-dependent effect of high glucose concentration on viability of notochordal cells and expression of matrix degrading and fibrotic enzymes. Int Orthop. 2013;37(6):1179-1186. doi:10.1007/s00264-013-1836-2
- 8 Park EY, Park JB. High glucose-induced oxidative stress promotes autophagy through mitochondrial damage in rat notochordal cells. Int Orthop. 2013;37(12):2507-2514. doi:10.1007/s00264-013-2037-8
- 9 Kong JG, Park JB, Lee D, Park EY. Effect of high glucose on stress-induced senescence of nucleus pulposus cells of adult rats. Asian Spine J. 2015;9(2):155-161. doi:10.4184/asj.2015.9.2.155
- 10 Kong CG, Park JB, Kim MS, Park EY. High glucose accelerates autophagy in adult rat intervertebral disc cells. Asian Spine J. 2014;8(5):543-548. doi:10.4184/asj.2014.8.5.543