Depression may be diagnosed if an individual experiences extreme sadness or despair that lasts for more than several days. Continuous, severe pain from degenerative disc disease and depression are closely linked in two ways:
- Severe pain from lumbar degenerative disc disease may understandably lead to depression
- Psychological distress, such as depression, is the second most significant risk factor for disability,1Mannion AF, Junge A, Taimela S, Müntener M, Lorenzo K, Dvorak J. Active therapy for chronic low back pain: part 3. Factors influencing self-rated disability and its change following therapy. Spine (Phila Pa 1976). 2001;26(8):920-929. doi:10.1097/00007632-200104150-00015 and may lead to pain or worsen existing pain
Close to half of all patients whose pain was severe enough to warrant spinal surgery also have depression, and the depression usually persists after surgery as well.2Jabłońska R, Ślusarz R, Królikowska A, Haor B, Antczak A, Szewczyk M. Depression, social factors, and pain perception before and after surgery for lumbar and cervical degenerative vertebral disc disease. J Pain Res. 2017;10:89-99. Published 2017 Jan 4. doi:10.2147/JPR.S121328 When both chronic pain and depression are present, it is essential to treat both the depression and the pain rather than just one or the other, as they are compounding conditions.
In This Article:
- Degenerative Disc Disease Treatment for Low Back Pain
- Exercise and Physical Therapy for Disc Disease Treatment and Pain Management
- Pain Medications for Degenerative Disc Disease Treatment
- Pain Management Techniques for Degenerative Disc Disease
- Treating Chronic Pain and Depression from Degenerative Disc Disease
Antidepressant Medications
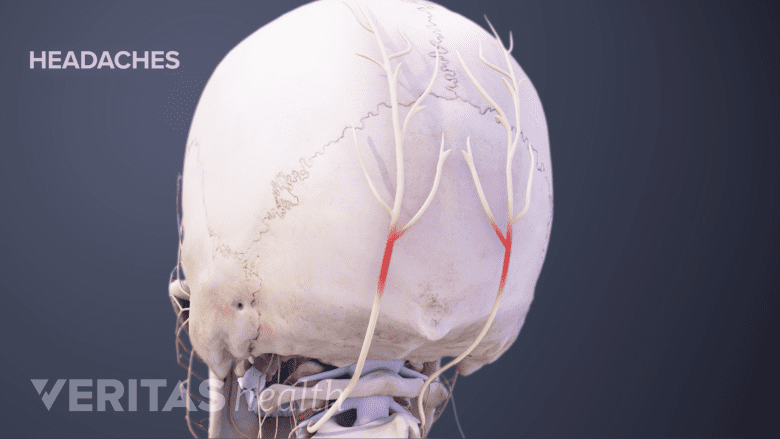
Headaches can be a common, temporary side effect of antidepressant medications.
Antidepressant medications also seem to have an anti-pain quality.3Urits I, Peck J, Orhurhu MS, et al. Off-label Antidepressant Use for Treatment and Management of Chronic Pain: Evolving Understanding and Comprehensive Review. Curr Pain Headache Rep. 2019;23(9):66. Published 2019 Jul 29. doi:10.1007/s11916-019-0803-z Specific classes of antidepressants used for chronic pain include:
- Tricyclic antidepressants (TCAs), such as imipramine (Tofranil)
- Serotonin and norepinephrine reuptake inhibitors (SNRIs), such as duloxetine (Cymbalta)
- Atypical antidepressants, such as bupropion (Wellbutrin)
These medications work by targeting and lowering the central sensitization of chronic lower back pain.4Urquhart DM, Wluka AE, van Tulder M, et al. Efficacy of Low-Dose Amitriptyline for Chronic Low Back Pain: A Randomized Clinical Trial [published correction appears in JAMA Intern Med. 2019 Mar 1;179(3):457]. JAMA Intern Med. 2018;178(11):1474-1481. doi:10.1001/jamainternmed.2018.4222 One pronounced side effect of antidepressants is an initial "hangover" effect (headaches, dizziness, or grogginess), but the effect tends to recede over time.
These medications may be used to treat only pain, or both pain and depression. In low doses, antidepressants may have a pain-relieving effect without altering the mood. In higher doses, antidepressants may help treat pain and depression.
Active Physical Therapy and Exercise
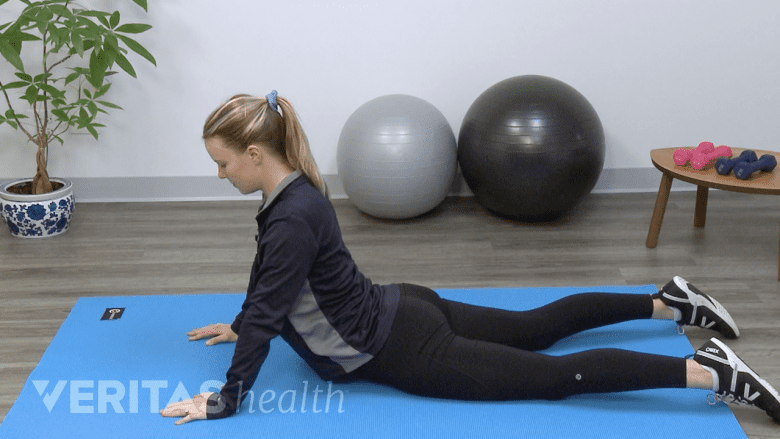
Gentle stretches promote flexibility and reduce muscle tightness in the lower back and legs.
Engaging in an exercise routine elevates the heart rate and may alleviate depression as well as chronic low back pain. Active exercise also releases endorphins, the body’s natural pain-relieving and “feel good” chemical, which helps with mood and pain reduction. Physical therapy is superior to exercises performed at home. The success of completing an exercise directed by a physical therapist, physiatrist, or other qualified health professional tends to reduce fear and provide confidence, and when correctly done an exercise program may significantly reduce pain.
See Physical Therapy for Low Back Pain Relief
Psychological Therapy
Psychological therapy is usually a core component of treatment for depression. Therapeutic approaches often have a neuroscientific or clinical basis. Examples include cognitive behavioral therapy, which may help treat the 90% of low back pain cases that do not have a clearly identifiable cause,5O'Sullivan PB, Caneiro JP, O'Keeffe M, et al. Cognitive Functional Therapy: An Integrated Behavioral Approach for the Targeted Management of Disabling Low Back Pain [published correction appears in Phys Ther. 2018 Oct 1;98(10):903]. Phys Ther. 2018;98(5):408-423. doi:10.1093/ptj/pzy022 and biofeedback, which may train the mind to influence the level of pain. This form of treatment can be individualized, altering the patient’s experience of pain using modifiable factors such as the coping response or the environmental triggers.
See 4 Tips to Help Cope With Chronic Pain and Depression
Sleep Treatments
With depression and chronic pain, sleep problems may complicate matters and make it more difficult for the patient to heal. If patients are not sleeping regularly, it makes it much more difficult to cope with the stress that chronic pain creates, which in turn may lead to more depression.
Antidepressant medications
A number of older-generation antidepressants (such as amitriptyline, nortriptyline, or imipramine) are used to treat sleep disorders and chronic pain. These drugs are usually:
- Well tolerated when used at night
- Prescribed in doses that are a fraction of the dose for treating depression
- Not addictive
The drugs are designed to restore sleep without changing the sleep cycle.
Other antidepressant medications may also be prescribed to help with sleep. For example, trazodone is commonly prescribed to help with sleep as it does not disturb the quality of sleep, is not considered addictive, and may help with mood and energy, as well as sleep.
Medical cannabis
Cannabis is a treatment option for chronic pain, and cannabis happens to have properties that improve disturbed sleep. The use of this drug as a medical treatment for sleep disorders6Sznitman SR, Vulfsons S, Meiri D, Weinstein G. Medical cannabis and insomnia in older adults with chronic pain: a cross-sectional study. BMJ Support Palliat Care. 2020;10(4):415-420. doi:10.1136/bmjspcare-2019-001938 and for chronic pain has been proven beneficial, but frequent use may develop drug tolerance and lead to increased difficulty falling and staying asleep.7Pranikoff K, Karacan I, Larson EA, Williams RL, Thornby JI, Hursch CJ. Effects of marijuana smoking on the sleep EEG. Preliminary studies. JFMA. 1973;60(3):28-31.,8Karacan I, Fernández-Salas A, Coggins WJ, et al. Sleep electroencephalographic-electrooculographic characteristics of chronic marijuana users: part I. Ann N Y Acad Sci. 1976;282:348-374. doi:10.1111/j.1749-6632.1976.tb49909.x,9Angarita GA, Emadi N, Hodges S, Morgan PT. Sleep abnormalities associated with alcohol, cannabis, cocaine, and opiate use: a comprehensive review. Addict Sci Clin Pract. 2016;11(1):9. Published 2016 Apr 26. doi:10.1186/s13722-016-0056-7
Some studies have shown that higher doses of medical cannabis over several years may have the added benefit of helping to stop or reduce opioid use.10Takakuwa KM, Hergenrather JY, Shofer FS, Schears RM. The Impact of Medical Cannabis on Intermittent and Chronic Opioid Users with Back Pain: How Cannabis Diminished Prescription Opioid Usage. Cannabis Cannabinoid Res. 2020;5(3):263-270. Published 2020 Sep 2. doi:10.1089/can.2019.0039,11Vigil JM, Stith SS, Adams IM, Reeve AP. Associations between medical cannabis and prescription opioid use in chronic pain patients: A preliminary cohort study. PLoS One. 2017;12(11):e0187795. Published 2017 Nov 16. doi:10.1371/journal.pone.0187795 Discontinuation of opioid use may alleviate sleep issues and depression because opioids tend to exacerbate depression12Cao M, Javaheri S. Effects of Chronic Opioid Use on Sleep and Wake. Sleep Med Clin. 2018;13(2):271-281. doi:10.1016/j.jsmc.2018.02.002 and sleep apnea or sleep-related breathing disorders. 13Marshansky S, Mayer P, Rizzo D, Baltzan M, Denis R, Lavigne GJ. Sleep, chronic pain, and opioid risk for apnea. Prog Neuropsychopharmacol Biol Psychiatry. 2018;87(Pt B):234-244. doi:10.1016/j.pnpbp.2017.07.014
- 1 Mannion AF, Junge A, Taimela S, Müntener M, Lorenzo K, Dvorak J. Active therapy for chronic low back pain: part 3. Factors influencing self-rated disability and its change following therapy. Spine (Phila Pa 1976). 2001;26(8):920-929. doi:10.1097/00007632-200104150-00015
- 2 Jabłońska R, Ślusarz R, Królikowska A, Haor B, Antczak A, Szewczyk M. Depression, social factors, and pain perception before and after surgery for lumbar and cervical degenerative vertebral disc disease. J Pain Res. 2017;10:89-99. Published 2017 Jan 4. doi:10.2147/JPR.S121328
- 3 Urits I, Peck J, Orhurhu MS, et al. Off-label Antidepressant Use for Treatment and Management of Chronic Pain: Evolving Understanding and Comprehensive Review. Curr Pain Headache Rep. 2019;23(9):66. Published 2019 Jul 29. doi:10.1007/s11916-019-0803-z
- 4 Urquhart DM, Wluka AE, van Tulder M, et al. Efficacy of Low-Dose Amitriptyline for Chronic Low Back Pain: A Randomized Clinical Trial [published correction appears in JAMA Intern Med. 2019 Mar 1;179(3):457]. JAMA Intern Med. 2018;178(11):1474-1481. doi:10.1001/jamainternmed.2018.4222
- 5 O'Sullivan PB, Caneiro JP, O'Keeffe M, et al. Cognitive Functional Therapy: An Integrated Behavioral Approach for the Targeted Management of Disabling Low Back Pain [published correction appears in Phys Ther. 2018 Oct 1;98(10):903]. Phys Ther. 2018;98(5):408-423. doi:10.1093/ptj/pzy022
- 6 Sznitman SR, Vulfsons S, Meiri D, Weinstein G. Medical cannabis and insomnia in older adults with chronic pain: a cross-sectional study. BMJ Support Palliat Care. 2020;10(4):415-420. doi:10.1136/bmjspcare-2019-001938
- 7 Pranikoff K, Karacan I, Larson EA, Williams RL, Thornby JI, Hursch CJ. Effects of marijuana smoking on the sleep EEG. Preliminary studies. JFMA. 1973;60(3):28-31.
- 8 Karacan I, Fernández-Salas A, Coggins WJ, et al. Sleep electroencephalographic-electrooculographic characteristics of chronic marijuana users: part I. Ann N Y Acad Sci. 1976;282:348-374. doi:10.1111/j.1749-6632.1976.tb49909.x
- 9 Angarita GA, Emadi N, Hodges S, Morgan PT. Sleep abnormalities associated with alcohol, cannabis, cocaine, and opiate use: a comprehensive review. Addict Sci Clin Pract. 2016;11(1):9. Published 2016 Apr 26. doi:10.1186/s13722-016-0056-7
- 10 Takakuwa KM, Hergenrather JY, Shofer FS, Schears RM. The Impact of Medical Cannabis on Intermittent and Chronic Opioid Users with Back Pain: How Cannabis Diminished Prescription Opioid Usage. Cannabis Cannabinoid Res. 2020;5(3):263-270. Published 2020 Sep 2. doi:10.1089/can.2019.0039
- 11 Vigil JM, Stith SS, Adams IM, Reeve AP. Associations between medical cannabis and prescription opioid use in chronic pain patients: A preliminary cohort study. PLoS One. 2017;12(11):e0187795. Published 2017 Nov 16. doi:10.1371/journal.pone.0187795
- 12 Cao M, Javaheri S. Effects of Chronic Opioid Use on Sleep and Wake. Sleep Med Clin. 2018;13(2):271-281. doi:10.1016/j.jsmc.2018.02.002
- 13 Marshansky S, Mayer P, Rizzo D, Baltzan M, Denis R, Lavigne GJ. Sleep, chronic pain, and opioid risk for apnea. Prog Neuropsychopharmacol Biol Psychiatry. 2018;87(Pt B):234-244. doi:10.1016/j.pnpbp.2017.07.014

