Obtaining a clinical diagnosis of the underlying cause of lower back pain, not merely a description of the symptoms, is important in guiding treatment.
The first step in the clinical diagnostic process is a detailed description of symptoms and medical history.
From this information, a doctor will usually be able to identify or at least narrow in on the cause of the pain. Further diagnostic testing may be indicated if the cause of the pain is unclear or for pre-surgical planning.
In This Article:
Patient History

A thorough medical history is an important diagnostic tool.
This initial consultation is to understand the individual’s medical history and symptoms, such as:
Information about current symptoms
- Is the pain better or worse at certain times of day, such as waking up or after work?
- How far does the pain spread?
- Are there other symptoms at the same time, such as weakness or numbness?
- What does the pain feel like—achy, sharp, tight, dull, hot, stinging?
Activity level
- How active or sedentary is one’s lifestyle? For example, does work require long hours sitting at a desk or standing at an assembly line?
- How many hours per day are spent sitting while watching TV or another device?
- How many hours and days per week are spent doing active exercise?
Sleep habits
- Generally, how many hours of sleep does the patient get?
- What sleep position is preferred?
- Is the sleep continuous or are there frequent wakings during the night?
Injuries
- Have there been any recent injuries?
- Has there been an injury in the past that might be relevant now?
- Are there daily stresses to the spine, such as job requirements?
Answers to these questions provide a fuller picture of the patient’s daily life, indicating more specific possibilities for low back pain. A medical history is often the most powerful tool for finding a diagnosis.
Physical Exam
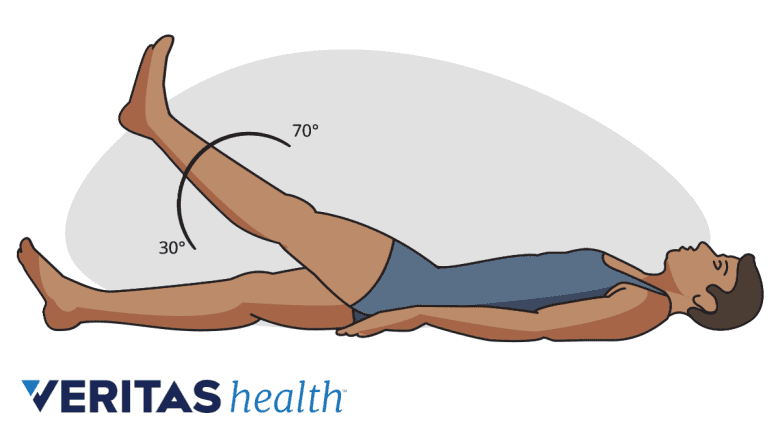
A positive straight leg raise test may be suggestive of a herniated disc.
The goal of a physical exam is to hone in on the likely cause of pain, and usually includes a combination of:
Palpation
A doctor will feel by hand (called palpating) along the lower back to locate any muscle spasms or tightness, areas of tenderness or swelling, or joint abnormalities.
Neurologic exam
This exam includes manual movement of the hip, knee, ankle movement, and big toe extension and flexion (movement forward and backward). Tests may include foot drop or other neurological deficits.
A sensory exam will includes reaction to light touch, a pinprick, or other senses around the lower back, hip, buttock, and legs.
Range of motion test
The patient may be asked to bend or twist in certain positions. These activities are done to look for positions that worsen or recreate pain and to see if specific movements are limited by discomfort.
Straight leg raise test
Also called the Laseque sign, this simple test involves the patient lying on their back and the doctor assists in raising one leg without bending it at the knee. If this movement induces or worsens pain (usually leg pain), it suggests a possible problem with a sciatic nerve root and possibly a lumbar herniated disc.
Diagnostic Imaging Tests

Imaging tests may be used to confirm the source of back pain.
A diagnostic imaging test may be used to confirm the diagnosis, provide more detailed information on the pathology, and/or for surgical planning. Tests used are:
An MRI, or Magnetic Resonance Imaging scan, provides a detailed image of spinal structures without using the radiation required with x-rays. An MRI of the spine detects abnormalities with soft tissues, such as muscles, ligaments, and intervertebral discs. An MRI might also be used to locate misalignments or joint overgrowth in the spine.
X-rays are used to look at the bones of the spine. X-rays show abnormalities, such as arthritis, fractures, bone spurs, or tumors.
A CT scan/myelogram is a type of X-ray that provides a cross-sectioned image of the spine. A CT scan (Computer Tomography) provides more detailed imagery from specific angles.
Spinal injections are used to confirm the source of the pain; if the anti-inflammatory and/or numbing agent injected provides pain relief, that structure is confirmed as the source of the pain. Injection outcomes are considered predictive of surgical outcomes.
When a full spinal workup does not result in a definitive diagnosis, it may be time to consider alternative causes of the pain. For example, an autoimmune disorder such as fibromyalgia, a gynecological cause such as an ovarian cyst, or an infection such as Lyme disease are all known to cause back pain, and each requires a different diagnostic approach.

