Some conditions can feel similar to cervical osteoarthritis, so it is imperative to see a doctor for an accurate diagnosis and effective treatment plan.
In This Article:
- Cervical Osteoarthritis (Neck Arthritis)
- Cervical Osteoarthritis Symptoms
- Diagnosing Cervical Osteoarthritis
- Cervical Osteoarthritis Treatment
- Cervical Facet Osteoarthritis Video
Initial Doctor Visit
In order to diagnose the cause of a patient’s neck pain, the doctor will likely start with the following:
Review patient’s medical history

A thorough medical history is an important step in diagnosing cervical osteoarthritis.
Many conditions can be ruled out simply by gathering a detailed list of the patient’s current symptoms, past medical history, and current lifestyle habits.
Perform a physical exam

A physical exam includes checking for abnormalities, weakness, and reflexes.
To further narrow down the list of possible neck pain causes, the doctor will palpate (feel) the patient’s neck for any abnormalities or tenderness, as well as test the neck for any noticeable weakness or reduced range of motion. If the patient has complained of symptoms radiating down the arm, the doctor will also likely perform Spurling’s test by gently applying pressure to the top of the head while bent to the side. Spurling’s test checks to see if compressing the cervical spine (temporarily) worsens or recreates the patient’s symptoms, which could indicate a pinched nerve.
If the doctor collects enough information to suspect cervical osteoarthritis, he or she will likely recommend starting the patient on a nonsurgical treatment program.
Advanced Diagnostic Techniques
If the medical history and physical exam do not give the doctor enough information, or if the initial treatment plan is not providing relief, advanced diagnostics might be requested. This could include one or more of the following:
X-ray
Using electromagnetic radiation, an X-ray (radiograph) of the spine can show good images of the bones and cartilage, and whether they are degenerating.
MRI scan

An MRI scan is a useful diagnostic tool that aids in the identification of nerve compression.
Using radio waves and a strong magnet, an MRI creates a series of detailed cross-sections of soft tissues and bones. An MRI scan does not show bones as well as an x-ray, but the MRI is better at showing soft tissues and can be useful if nerve compression is suspected.
Diagnostic injections
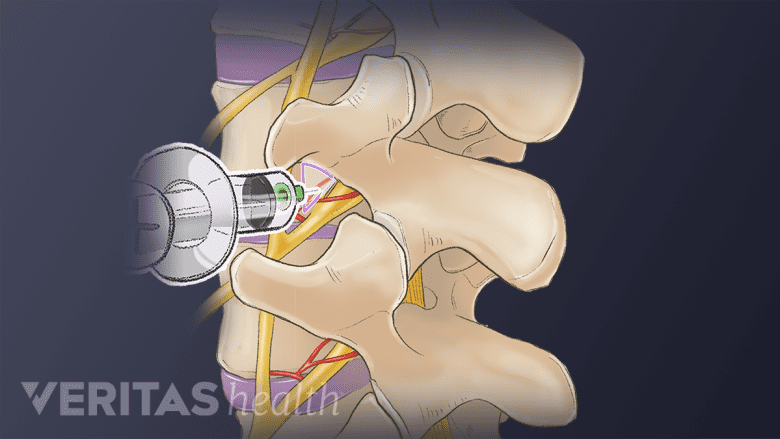
A cervical facet injection may provide temporary pain relief by reducing inflammation.
A certified medical professional can use x-ray guidance to administer an injection that delivers medicine (a steroid and/or anesthetic) directly into or near the cervical facet joint. A cervical facet injection goes into the joint, whereas a medial branch nerve block goes near the joint and delivers medicine to the small nerves that carry pain signals from the facet joint to the brain. While these types of injections can bring temporary relief of a few weeks or a few months, they are more of a diagnostic tool to see if the facet joint is the source of pain. Some studies indicate that the medial branch nerve blocks tend to offer longer-lasting relief than facet joint injections in the cervical spine.1Boswell MV, Colson JD, Sehgal N, Dunbar EE, Epter R. A systematic review of therapeutic facet joint interventions in chronic spinal pain. Pain Physician. 2007; 10:229-53.
See Selective Nerve Root Block Injections
Electrodiagnostic testing

Electromyography monitors muscle and nerve function by tracking electrical activity in muscles.
Various tests can be done to check nerve function. Two tests commonly done together include an electromyography (EMG), which measures electrical activity in muscles, and a nerve conduction study, which measures how fast nerves are sending signals. A problem detected during electrodiagnostic testing could indicate a nerve in the neck is being compressed due to spinal degeneration.
This is not a complete list of advanced diagnostic techniques. Many other possibilities exist, including CT scan with myelogram.
Advanced diagnostic testing tends to be expensive and inconvenient, so they are typically not used unless other diagnostic options have been exhausted.
Diagnosis Can Be Elusive
There is no one test that can be used to diagnose cervical osteoarthritis. Instead, the doctor will collect as much relevant information as possible to exclude certain conditions and narrow down the list to eventually reach an accurate diagnosis.
Furthermore, it is important to remember that imaging studies, such as x-rays, MRI scans, or CT scans, may show results that do not match the patient’s symptoms. For example, an MRI scan may indicate severe spinal degeneration but the patient’s symptoms may not seem to stem from that area. Likewise, a patient may have severe symptoms but the MRI might not show significant spinal degeneration.
As such, it is important for any treatment plan to address the patient’s stated symptoms as opposed to solely relying on an imaging study or any other diagnostic test.
- 1 Boswell MV, Colson JD, Sehgal N, Dunbar EE, Epter R. A systematic review of therapeutic facet joint interventions in chronic spinal pain. Pain Physician. 2007; 10:229-53.

