While Klippel-Feil syndrome (KFS) is a congenital bone condition that is present from birth, it is not always noticed at that time. Many factors can affect whether Klippel-Feil syndrome (KSF) is diagnosed at a young age or not.
Why an Early KFS Diagnosis May Be Missed
In cases where a KFS diagnosis is delayed for years or decades, it is usually for one or both of the following reasons:
- Signs are initially absent or minor. If the neck is not noticeably shorter or limited in mobility, it is unlikely for KFS to be diagnosed. As someone with KFS gets older, he or she may notice small issues, such as less of an ability to look down compared to others, or increasing amounts of headaches and/or neck pain. Even so, these signs and symptoms might be dismissed as minor, normal, and/or simply not pursued, which can allow the condition to remain undiagnosed.
- Other conditions need more immediate medical attention. In many cases, other malformations are also present with KFS. If another malformation or condition is serious or even life threatening, such as a heart defect or spinal cord compression, that condition is likely to be diagnosed and treated without officially diagnosing KFS alongside it.
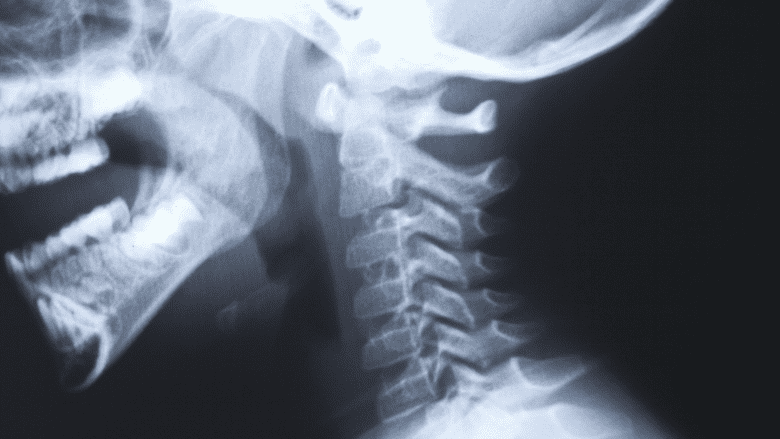
Sometimes a person is not diagnosed with KFS until an injury occurs that requires x-rays of the neck, such as from a motor vehicle accident.
In This Article:
- What to Know About Klippel-Feil Syndrome
- Klippel-Feil Symptoms and Associated Conditions
- Klippel-Feil Syndrome Diagnosis
- Klippel-Feil Syndrome Treatment
Importance of Diagnosing KFS
The earlier that KFS can be diagnosed, the better the condition can be treated and managed. Some specific benefits of an early KFS diagnosis include:
- Determining the severity and risks. If imaging of the cervical spine shows exposure of the spinal cord or any other vulnerabilities in the vertebral column, certain activities may need to be avoided. In cases where the cervical spine is found to be vulnerable, an injury that would be minor for most people could instead result in serious complications, including paralysis or death.
- Potentially treating some problems before they worsen or develop. Some cases of KFS may significantly progress while others may not. For example, if a deformity in the cervical and/or thoracic spine is starting to progress, surgery may be advised to stabilize the spine and prevent the problem from becoming worse. Waiting too long could limit the effectiveness of such a surgery.
How KFS Is Diagnosed
X-rays are helpful in diagnosing Klippel-Feil syndrome.
An official KFS diagnosis typically involves the following:
- Medical history. The patient’s medical background is carefully reviewed, including any current signs and symptoms, when they started, and any other conditions that might be present and/or run in the family.
- Physical exam. The doctor observes and/or palpates the head, neck, shoulders, spine, and any other relevant areas of the body to determine where abnormalities may be present.
- Imaging studies. An x-ray and/or CT scan are likely to be taken to examine the bones. An MRI is likely to be done to examine soft tissues and determine whether any nerve and/or spinal cord compression is present.
See Introduction to Diagnostic Studies for Back and Neck Pain
- Genetic testing. A DNA sample may be taken and examined to see if there are mutations in any genes, such as GDF3, GDF6, or MEOX1, which are commonly altered in KFS.
If at least 2 cervical vertebrae are fused and other aspects of the exam signal that the condition is congenital (from birth), Klippel-Feil syndrome is diagnosed.