Ankylosing spondylitis is a form of arthritis that can cause flares of burning pain in the spine. It typically develops in the lower back and hips but gradually progresses up toward the neck over time. Some people may go years and only deal with occasional episodes of intense spinal pain. Others might have frequent flare-ups as the disease continues to spread and get worse.
While neck pain is not the first symptom to appear with ankylosing spondylitis—and sometimes never develops—it can be a troubling symptom, as it typically appears when the disease has become more advanced.
This article examines how to tell when neck pain may be caused by ankylosing spondylitis and how it can be treated.
In This Article:
Ankylosing Spondylitis Symptoms
In ankylosing spondylitis, inflammation, and calcification can spread up the spine, making it stiff and painful.
Ankylosing spondylitis and its associated symptoms tend to start slowly. Common early symptoms may include:
- Spinal pain and stiffness. This pain can range from a mild ache to a sharp burning sensation. Ankylosing spondylitis is typically first noticed in the lower back (lumbar spine) or buttocks (sacroiliac joints between the sacrum and pelvis).
- Pain that worsens with rest. Exercise or activity may reduce the inflammatory pain of ankylosing spondylitis, but inactivity can exacerbate it. In fact, the pain can intensify during sleep, which sometimes leads to waking up in the night.
Symptoms that may develop later could include:
- Sensitivity to light. During a flare-up, vision may become blurry and bright lights could cause eye pain.
- Lethargy. Individuals may feel tired or easily fatigued, even after trying to get adequate rest.
- Pain in other joints. In addition to spreading up the spine toward the neck, ankylosing spondylitis can also affect the shoulders, knees, hips, fingers, and other joints.
- Chest pain. Cartilage inflammation between the sternum (breastbone) and ribs can cause intense pain that could be mistaken for a cardiac event.
- Loss of spinal mobility. In rare cases, ankylosing spondylitis can eventually cause so much damage to the spine’s intervertebral discs and facet joints that vertebral bones start to fuse together.
Watch: Ankylosing Spondylitis Video
Several other ankylosing spondylitis symptoms are also possible.
How Ankylosing Spondylitis Causes Neck Pain
Ankylosing spondylitis can cause neck pain and stiffness in a few different ways:
Inflammation of the cervical spine
Enthesitis causes inflammation in the cervical spine at regions where ligaments or tendons attach to bone.
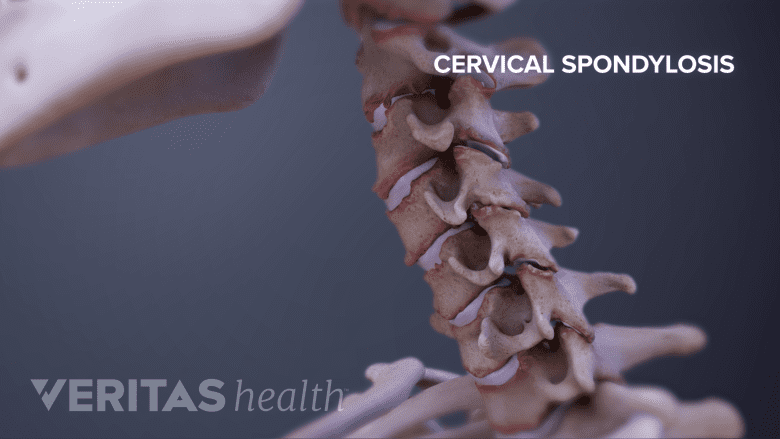
Ankylosing spondylitis causes enthesitis, which is inflammation and the formation of scar tissue where ligaments, tendons, and other soft tissues attach to a bone. This disease process, which initially affects the lumbar spine, can eventually affect the cervical spine. For example, enthesitis can lead to more bone formation within a facet joint in the cervical spine, which continues the cycle of more inflammation and more stiffness. Nearby discs may also start to calcify (turn to bone) and stiffen as part of this process.
Poor posture
While ankylosing spondylitis usually first causes pain and swelling in the lower back and hips, postural changes due to symptoms in these areas can also contribute to neck pain before the condition spreads to the cervical spine. Spinal degeneration in the middle and lower back can cause painful and stiffening spinal joints, which can in turn lead to reduced activity levels and weakened muscles. If muscles weaken and/or tighten in the neck, upper back, and chest, or if the thoracic spine starts curving forward even more (kyphosis) due to degenerative changes, then neck muscles and cervical spine joints can become stressed and painful while working harder to support the head.
See How Poor Posture Causes Neck Pain
More commonly, a person who has ankylosing spondylitis in the early stages or only in the lower back can develop unrelated neck pain from a variety of other causes, such as from overuse or sleeping on it wrong.
Increased Risk for Spinal Fractures
For a patient with advanced ankylosing spondylitis, autofusion of the spine’s motion segments can lead to long levers of fused spinal segments that increase stress in the spine. This is especially important with traumatic events or falls. Stress concentrates through the stiff segments and fractures can occur. In particular, the disc space is the weakest area and most vulnerable to fractures.
Even after a minor trauma, an ankylosing spondylitis patient in pain must be thoroughly evaluated to avoid missing fractures. CT scans are indicated to identify the fractures and surgical stabilization is often required to prevent neurologic injury.