The C2-C5 spinal motion segments comprise three individual segments: C2-C3, C3-C4, and C4-C5. This group of motion segments starts with the C2 vertebra near the top of the cervical spine and ends in the mid-cervical spine at the C5 vertebra. The C2-C5 motion segments contribute the most to the mid-range of motion during the neck’s forward and/or backward movements. C4-C5 is typically more mobile compared to other motion segments between C2-C5.1Anderst WJ, Donaldson WF 3rd, Lee JY, Kang JD. Cervical motion segment percent contributions to flexion-extension during continuous functional movement in control subjects and arthrodesis patients. Spine (Phila Pa 1976). 2013;38(9):E533–E539. doi:10.1097/BRS.0b013e318289378d
The lower cervical spine (C5-C7) is typically injured more often compared to C2-C5. However, the C2-C5 motion segments are also susceptible to injury and can cause pain due to degeneration, disc herniation, trauma, and neurological injury.
See All About the C5-C6 Spinal Motion Segment and All About the C6-C7 Spinal Motion Segment
In This Article:
- All About the C2-C5 Spinal Motion Segments
- C2-C5 Treatment
- Spinal Motion Segment: C2-C5 Animation
Anatomy of the C2-C5 Spinal Motion Segments
The C2-C5 motion segments include the following structures:
Vertebrae and joints from C2 through C5

The C2-C5 segments provide support and mobility for the middle part of the cervical spine.
The vertebrae in the C2-C5 motion segments are held together with ligaments and connected by paired facet joints running down the back of the spine. These joints are synovial joints that contain articulating cartilage to help facilitate smooth gliding movements between adjacent vertebrae.
Watch Cervical Vertebrae Anatomy Animation
Intervertebral discs

The cervical discs facilitate neck movements and act like shock absorbers.
Between each vertebral body, there is a disc made up of a thick fibrous outer ring (annulus fibrosus) with a gel-like core (nucleus pulposus). This disc provides cushioning and shock-absorbing functions to protect the vertebrae from grinding against each other during neck movements, while also allowing movement in all directions.
Watch Cervical Disc Anatomy Animation
Spinal nerves

Each spinal nerve has its own anterior and posterior roots.
Within each motion segment, spinal nerves exit the spinal cord through small bony openings on the left and right sides of the spinal canal called the intervertebral foramina. These foramina are situated between two adjacent vertebrae.
Each spinal nerve receives sensation from specific areas of skin—its dermatome; and controls specific groups of muscles—its myotome:
- The C3 spinal nerve dermatome typically includes the skin over parts of the upper neck. The C3 myotome commonly includes certain neck muscles that help bend the neck forward.
- The C4 spinal nerve dermatome usually includes parts of skin over the shoulder. The C4 myotome includes certain muscles that help in shoulder movements.
- The C5 spinal nerve dermatome typically includes parts of skin over the shoulder, upper arm, and forearm. The C5 myotome includes certain muscles that help in shoulder movements.
Branches of the C3, C4, and C5 spinal nerves form the phrenic nerve that innervates the diaphragm, enabling breathing.
Within the spinal canal of each of these motion segments, the spinal cord is protected by the vertebral bodies in front and vertebral arches at the back.
Common Problems at C2-C5
Typically, in the C2-C5 motion segments, the C2 and/or C5 vertebrae are at a higher risk of injury and/or disease.2Torlincasi AM, Waseem M. Cervical, Injury. [Updated 2018 Oct 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-.Available from: https://www.ncbi.nlm.nih.gov/books/NBK448146/. Common problems in the C2-C5 motion segments are:
Spondylosis
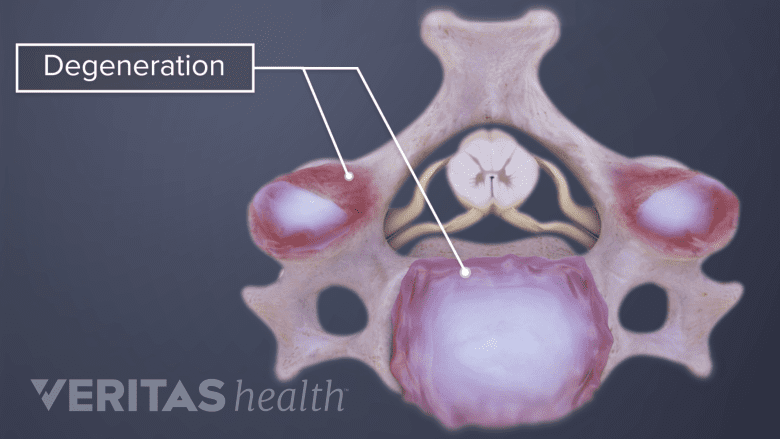
Spondylosis refers to degeneration of the spinal tissues.
The C2 and C5 vertebrae are commonly affected by spondylosis or degenerative conditions. As a result, the growth of bone spurs or osteophytes may eventually compress a nerve root or the spinal cord.
Watch Cervical Spondylosis with Myelopathy Animation
Congenital stenosis
The C5 vertebra is at a higher risk of stenosis occurring from birth compared to the other vertebrae in C2-C5 motion segments.3Binder AI. Cervical spondylosis and neck pain. BMJ. 2007;334(7592):527-31.
Fracture
The vertebrae from C2 through C5 may fracture or dislocate as a result of trauma from falls, motor vehicle accidents, or whiplash injuries.
Disc herniation

Herniated discs cause pain by pressing on the nerve.
The intervertebral disc may get herniated, eventually irritating or compressing an adjacent nerve root.
See Cervical Herniated Disc Symptoms and Treatment Options
Phrenic nerve damage
Blunt or penetrating trauma, or spondylosis in the C2-C5 motion segments may damage the phrenic nerve, causing breathing problems.
Rarely, tumors and infections may affect the C2-C5 motion segments.
Common Symptoms and Signs Stemming from C2-C5

Issues with the C2-C5 vertebrae can cause numbness in the forearm and hand.
Pain from C2-C5 may occur suddenly after an injury or may develop over time, such as in case of degeneration. Symptoms are usually felt in the head, neck, shoulder and/or arms.
Common symptoms stemming from C2-C5 may include one or more of the following:
- Pain of moderate to severe intensity may be felt in the neck, shoulder, and/or upper arms. The pain may also radiate from the upper neck into the back of the head causing cervicogenic headache. The pain may be aggravated by neck and/or arm movements.
- Numbness in one or more parts of the forearm, hand, and/or one or more fingers.
- Weakness in the shoulder, elbow, and/or wrist; commonly affecting the motion of these joints.
- Difficulty in breathing or inability to breathe may result if the phrenic nerve is damaged.
Spinal cord compression within the C2-C5 spinal motion segments may cause pain, weakness, or paralysis in the arms and/or legs. There may be loss of bowel and bladder control in some cases.
Typically, nonsurgical treatments are tried first when treating pain stemming from the C2-C5 motion segments, with the exception of those stemming from spinal cord compression as described above. If pain persists despite 3 to 6 months of nonsurgical treatments, or if numbness and/or weakness continues to worsen, surgery may be considered.
- 1 Anderst WJ, Donaldson WF 3rd, Lee JY, Kang JD. Cervical motion segment percent contributions to flexion-extension during continuous functional movement in control subjects and arthrodesis patients. Spine (Phila Pa 1976). 2013;38(9):E533–E539. doi:10.1097/BRS.0b013e318289378d
- 2 Torlincasi AM, Waseem M. Cervical, Injury. [Updated 2018 Oct 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-.Available from: https://www.ncbi.nlm.nih.gov/books/NBK448146/.
- 3 Binder AI. Cervical spondylosis and neck pain. BMJ. 2007;334(7592):527-31.

