Conditions affecting the T12-L1 spinal motion segment are usually treated with nonsurgical methods. Surgery may be recommended for abdominal or mid-back symptoms that continue to worsen or do not improve despite these treatments, or in case of medical emergencies, such as complex fractures or spinal cord compression.
In This Article:
Non-surgical Treatments for T12-L1
Initial treatments for T12-L1 symptoms include:
Medication
Over-the-counter or prescription medications are used to manage inflammation and/or pain.
- Nonsteroidal anti-inflammatory drugs (NSAIDs) are recommended to reduce inflammation in conditions such as muscle strains, ligament sprains, and nerve root inflammation from damaged discs.
- NSAIDs are available as oral tablets (eg, Advil) and topical ointments (eg, Voltaren), and can be purchased over the counter or with a prescription.
- Oral NSAIDs are not suitable for all patients due to significant potential risks, such as gastric irritation and/or bleeding, and cardiac problems.
- NSAIDs can potentially slow bone healing and are avoided during vertebral fractures or procedures like spinal fusion that require bone healing or fusion.
- Oral steroids, such as methylprednisolone and prednisone, may be prescribed to control inflammation and pain.
- Steroids are prescribed for short courses and start at a high dose, quickly tapering down to a lower dose, and discontinuing the medication within a period of 1 to 2 weeks.
- Steroids are not indicated when certain co-occurring medical conditions, such as diabetes, osteoporosis, or heart disorders, are present.
- Long-term use of steroids has significant risks, such as damaging bone health and slowing down natural healing processes.
- Opioids, such as tramadol, may be prescribed for severe, debilitating pain from vertebral fractures or other serious injuries.
- Opioids are only recommended for short-term use, such as 1 to 2 weeks.
- Opioid pain medications carry significant risks, such as addiction, drowsiness, constipation, vomiting, and nausea.
- Muscle relaxants, such as baclofen and diazepam, regulate muscle contraction (tightening) to reduce pain and discomfort caused by muscle spasms and stiffness.
- Muscle relaxants are recommended for short-term use, such as 1 to 2 weeks.
- Potential side effects and risks of muscle relaxants include drowsiness, headache, gastric symptoms, and cardiac (heart) symptoms.
It is always recommended to take medications under the guidance and supervision of a qualified medical professional.
Back brace
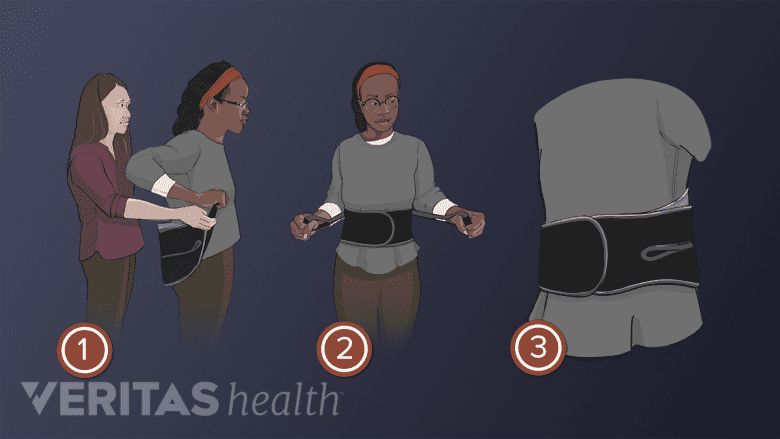
A brace immobilizes and protects the thoracolumbar area during the initial week or two of an acute injury, such as a fracture, or while recovering from surgery. Immobilization helps promote healing of the vertebrae and surrounding soft tissues such as ligaments and blood vessels.
See Using a Back Brace for Lower Back Pain Relief
Physical therapy
Guided physical therapy for the T12-L1 motion segment typically involves a 4 to 8-week structured program followed by ongoing home exercises. The exercises focus on the abdominal and core muscles and consist of stretching and strengthening techniques that aim to:
- Improve function in the upper and lower back
- Improve the range of motion
- Improve balance and prevent falls
These exercises promote healing within the thoracolumbar junction and offer long-term pain relief.
See Physical Therapy for Low Back Pain Relief
Manual manipulation and chiropractic adjustment
Manipulation of the thoracolumbar segment through chiropractic adjustment may help relieve pain stemming from T12-L1 (assuming there is no fracture, instability, or significant osteoporosis).
Massage therapy
Therapeutic massage is used to relieve muscle spasms and increase blood flow to the painful tissues, which may help healing by bringing nutrients and oxygen to these tissues.
Massages are typically considered for pain caused by muscle and ligament problems and are usually done in combination with physical therapy and exercise.
See Massage Therapy for Lower Back Pain
Heat and cold therapy
Applying a heating pad or soaking in a warm bath, relaxes the muscles and improves blood flow and healing in the upper and lower back. Heat therapy tends to be most beneficial before engaging in physical activity or exercise, and before going to bed.
The use of ice packs for cold therapy reduces pain and inflammation and is beneficial to calm activity-related inflammation after exercise sessions or physical activity.
A clean cloth or towel must be placed between the heat or ice pack and the skin to avoid burns or skin damage. Generally, application should be limited to 20 minutes at a time with a break of at least 2 hours before reapplying the pack.
Watch Should I Use Ice or Heat for My Lower Back Pain?
Injection Treatments for T12-L1
Injections may be considered in the following cases:
- For pain relief to help advance physical therapy.
- To manage ongoing symptoms after trying several combinations of non-surgical methods.
- As a diagnostic tool to confirm if the T12 nerve root is the cause of pain before surgery is considered. This type of diagnostic injection is called a selective nerve block.
Common injection treatments for T12-L1 are listed below.
Epidural steroid injections
Steroids injected directly into the spinal epidural space decrease inflammation and reduce the sensitivity of nerve fibers to pain, generating fewer pain signals. These injections are more effective in treating inflammatory causes of pain, such as pain from inflammatory proteins leaking out of a herniated or degenerated disc.
See Lumbar Epidural Steroid Injections
Radiofrequency ablation
This type of procedure does not inject medication into the spine; rather, a probe is inserted into the spine to create a heat lesion on a pain-transmitting nerve by heating it, thereby eliminating the pain signals. Ablation techniques for T12-L1 include radiofrequency ablation (RFA).
Surgical Treatments for T12-L1
There are several types of surgeries to treat pain and neurologic deficits stemming from the thoracolumbar junction.
Decompression surgeries
These surgeries aim to relieve pressure on a nerve root, such as from a herniated disc or bone spur, or the spinal cord, and include:
- Microdiscectomy: A small part of the disc material near the nerve root is taken out. A portion of the bone adjacent to the nerve root may also be trimmed to relieve compression.
- Laminectomy: A part or all of the lamina (area of bone at the back of the vertebra) is removed to provide more room for the cauda equina.
- Foraminotomy: The opening for the spinal nerve root (intervertebral foramen) is enlarged by trimming bony overgrowth, relieving compression.
- Facetectomy: The facet joints are trimmed to relieve compression of nerve roots.
Surgeons may perform more than one procedure at a time. For example, a laminoforaminotomy is when a laminectomy procedure is done along with a foraminotomy.
Most of these procedures are performed on an outpatient basis with minimally invasive techniques.
Interbody fusion
The damaged disc is removed and a bone graft implant is placed in between the T12 and L1 vertebrae. Sometimes additional bone or metal implants are used to ensure stability and fusion of this segment eliminating any motion in the T12-L1 segment.
Spinal cord stimulation
For some types of chronic, unresolved T12-L1 pain, spinal cord stimulation (SCS) may be an option. In SCS, a small device called a spinal cord stimulator is surgically implanted near the spine. The device generates electrical impulses to disrupt the pain signals from this segment before they reach the brain.
Spinal cord stimulation involves an initial trial period where the treatment is tested for effective pain relief before the stimulator is surgically implanted in the body.
Watch Spinal Cord Stimulation for Chronic Back Pain Video
A small risk of serious complications, such as infection, nerve injury, or excessive bleeding is possible with spinal surgeries. It is advisable to discuss the benefits, risks, and alternatives of surgery with a surgeon and understand the possible complications or long-term implications if surgery is not performed.

