Failed back surgery syndrome (FBSS) can be managed with nonsurgical and surgical treatments. A series of nonsurgical treatments are tried first for several months before invasive treatments are considered.
The development and treatment of FBSS, in general, is challenging for both patients and doctors and requires a systematic approach to diagnose and treat the underlying cause of pain. The primary goal of failed back surgery treatment is to reduce pain, improve the patient’s quality of life, and restore as much function as possible.1Orhurhu VJ, Chu R, Gill J. Failed Back Surgery Syndrome. [Updated 2022 May 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK539777/
In This Article:
- Failed Back Surgery Syndrome (FBSS): What It Is and How to Avoid Pain after Surgery
- Failed Spinal Fusion Surgery
- Failed Lumbar Decompression Back Surgery
- Scar Tissue and Pain After Back Surgery
- Treatment Options for Pain After Back Surgery
Medications
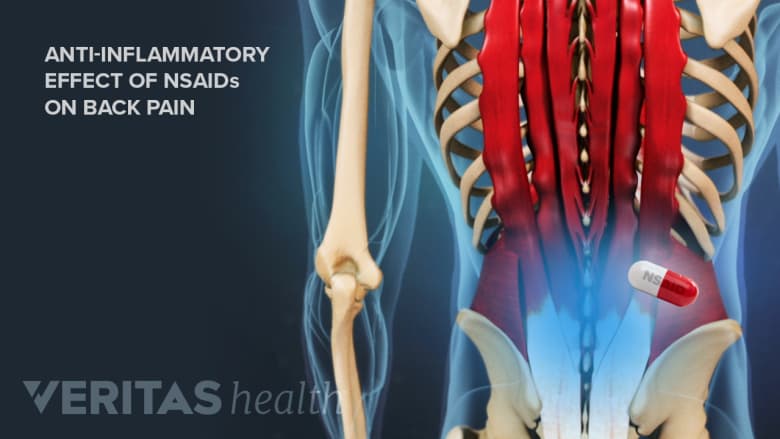
The anti-inflammatory effect of NSAIDs can help reduce post-surgical pain and discomfort associated with FBSS.
Oral medications for FBSS typically include nonsteroidal anti-inflammatory drugs (NSAIDs), opioid analgesics, anticonvulsant drugs, and antidepressants. These medications act by reducing inflammation and swelling or blocking pain signals to the brain. The dosage these medications needed for FBSS treatment typically requires a doctor's prescription.1Orhurhu VJ, Chu R, Gill J. Failed Back Surgery Syndrome. [Updated 2022 May 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK539777/
Physical Therapy
Guided physical therapy includes a series of exercises formulated by the therapist based on the patient's condition.
Guided physical therapy is a part of almost every treatment program for FBSS. The goals of physical therapy in treating FBSS are to increase muscle strength and improve the range of motion in the lower back. These goals are achieved through a series of exercises specially formulated by the therapist based on the patient's strengths and limitations.1Orhurhu VJ, Chu R, Gill J. Failed Back Surgery Syndrome. [Updated 2022 May 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK539777/
Massage and Manual Therapy
Hands-on manual therapies, such as massage and instrument-assisted soft tissue mobilization techniques, help break down and loosen scar tissue and adhesions under the skin and facilitate healing through the formation of new cells and fibers, such as collagen.
Spinal Cord Stimulation (SCS)

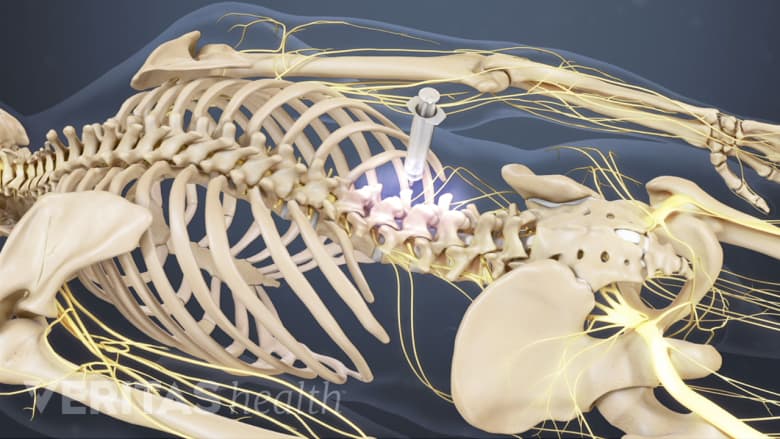
Electric signals from a spinal cord stimulator help distract the pain signals, thereby reducing pain.
SCS is a procedure in pain management where controlled, pulsed electric signals are passed near the spinal cord to distract the pain-transmitting nerves and control back pain. The electric signals are generated through a device, which is implanted in the patient’s back.1Orhurhu VJ, Chu R, Gill J. Failed Back Surgery Syndrome. [Updated 2022 May 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK539777/
The effectiveness of spinal cord stimulation can be tested in a trial phase, and if the results are favorable, permanent implantation can be performed.1Orhurhu VJ, Chu R, Gill J. Failed Back Surgery Syndrome. [Updated 2022 May 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK539777/
It is important to note that research on spinal cord stimulation treatment for chronic back pain is currently inconclusive and further long-term studies are needed to establish the safety and efficacy of SCS.2Traeger AC, Gilbert SE, Harris IA, Maher CG. Spinal cord stimulation for low back pain. Cochrane Back and Neck Group, ed. Cochrane Database of Systematic Reviews. 2023;2023(3). doi:10.1002/14651858.CD014789.pub2
Injection Treatments
Limited research indicates that spinal injections may provide pain relief in failed back surgery. Common injections include:
Adhesiolysis: an injection treatment to break down scar tissue
Adhesiolysis is an injection treatment that helps break down or dissolve scar tissue.
Adhesiolysis is a minimally invasive injection treatment where a physician injects a medicated solution, such as a steroid, saline, or hyaluronidase into the area of epidural scarring with the goal of breaking down or dissolving the scar tissue.3Manchikanti L, Manchikanti KN, Gharibo CG, Kaye AD. Efficacy of Percutaneous Adhesiolysis in the Treatment of Lumbar Post Surgery Syndrome. Anesth Pain Med. 2016;6(2):e26172. Published 2016 Mar 7. doi:10.5812/aapm.26172v2 A physiatrist, neurologist, or orthopedic surgeon with training in adhesiolysis may administer this injection.
Based on the extent and severity of the scar tissue and the general health of the patient, adhesiolysis treatment may take one session or several sessions over a period of a few days to complete. The procedure may be repeated after a few weeks if needed. Adhesiolysis may be recommended when nonsurgical treatments and physical therapy don’t provide pain relief from post-surgical scar tissue.4Cho JH, Lee JH, Song KS, et al. Treatment outcomes for patients with failed back surgery. Pain Physician. 2017;20(1):E29-E43.,5Hossieni B, Dadkhah P, Moradi S, Hashemi SM, Safdari F. The Results of Treating Failed Back Surgery Syndrome by Adhesiolysis: Comparing the One- and Three-Day Protocols. Anesth Pain Med. 2017;7(5):e60271. Published 2017 Aug 22. doi:10.5812/aapm.60271
Radiofrequency ablation: a nerve treatment to control pain
Radiofrequency ablation (RFA), also called radiofrequency neurotomy is a procedure that involves heating a part of a pain-transmitting nerve with a radiofrequency needle to create a heat lesion.
Once the RFA lesion is created, the pain-transmitting ability of the nerve fibers is lost and pain signals from the anatomical source do not reach the brain. The effects of RFA may last for a few months to years, after which the nerve usually regenerates, and the pain may or may not return (the procedure may be repeated in some cases).
Epidural steroids: an injection to control inflammation around the spinal canal

Epidural steroid injections may be administered through different approaches.
Epidural steroid injections deposit steroids and/or other medications in the epidural space of the spine. The epidural space contains nerves, blood vessels, and fat; and surrounds the dura, a sac around the spinal cord.
The steroids injected into the epidural space disperse into the nerve endings and other tissues, spreading the medication into these areas and relieving pain.
Revision Surgery

If the FBSS symptoms progressively worsen, revision surgery may be indicated.
Revision surgery for failed back surgery syndrome is considered when:
- Nonsurgical and minimally invasive pain management treatments have been tried for several months with no improvement in pain
- There’s a gradual worsening of symptoms
- Symptoms such as bowel/bladder impairment, severe motor weakness, or progressive neural deficit indicating a serious medical condition are present
- Radiographic and imaging tests confirm a failure of fusion (pseudoarthrosis), spinal instability, spinal imbalance, and/or new/recurrent disc herniation—which co-relates with the patient's post-surgical pain symptoms6Assaker R, Zairi F. Failed back surgery syndrome: To re-operate or not to re-operate? A retrospective review of patient selection and failures. Neurochirurgie. 2015;61:S77-S82. doi:10.1016/j.neuchi.2014.10.108
Revision surgeries may include spinal fusion, spinal realignment surgery, lumbar decompression, or disc replacement surgery depending on the cause of pain.
It is important to note that revision surgery will not guarantee a resolution of symptoms. A detailed discussion with the surgeon about the potential risks, benefits, and surgical alternatives is important before considering a revision surgery.
- 1 Orhurhu VJ, Chu R, Gill J. Failed Back Surgery Syndrome. [Updated 2022 May 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK539777/
- 2 Traeger AC, Gilbert SE, Harris IA, Maher CG. Spinal cord stimulation for low back pain. Cochrane Back and Neck Group, ed. Cochrane Database of Systematic Reviews. 2023;2023(3). doi:10.1002/14651858.CD014789.pub2
- 3 Manchikanti L, Manchikanti KN, Gharibo CG, Kaye AD. Efficacy of Percutaneous Adhesiolysis in the Treatment of Lumbar Post Surgery Syndrome. Anesth Pain Med. 2016;6(2):e26172. Published 2016 Mar 7. doi:10.5812/aapm.26172v2
- 4 Cho JH, Lee JH, Song KS, et al. Treatment outcomes for patients with failed back surgery. Pain Physician. 2017;20(1):E29-E43.
- 5 Hossieni B, Dadkhah P, Moradi S, Hashemi SM, Safdari F. The Results of Treating Failed Back Surgery Syndrome by Adhesiolysis: Comparing the One- and Three-Day Protocols. Anesth Pain Med. 2017;7(5):e60271. Published 2017 Aug 22. doi:10.5812/aapm.60271
- 6 Assaker R, Zairi F. Failed back surgery syndrome: To re-operate or not to re-operate? A retrospective review of patient selection and failures. Neurochirurgie. 2015;61:S77-S82. doi:10.1016/j.neuchi.2014.10.108

