A single-level cervical fusion involves two adjacent vertebrae in the cervical spine being fused together. While it is a relatively safe and routine procedure, it is still major surgery. Patients are correct to ask many questions before committing to it, including how neck mobility might be affected.
In This Article:
- How Much Neck Mobility Is Lost After Fusion Surgery?
- Neck Mobility After a Single-Level Cervical Fusion
- Neck Mobility After a Multilevel Cervical Fusion
What Happens During a Single-Level Cervical Fusion?
ACDF involves disc removal and vertebral fusion.
When a patient undergoes a single-level cervical fusion surgery, it is typically a two-part process:
- Decompression. Surgeon removes the intervertebral disc between adjacent vertebrae, as well as any other structures that might be irritating a spinal nerve or the spinal cord, such as bony overgrowths (bone spurs).
- Fusion. After the decompression part of the surgery, that spinal level needs to be stabilized. The surgeon instruments the two adjacent vertebrae and adds bone graft to promote bone growth and ultimately a solid fusion between the two vertebrae.
The surgery is termed an anterior cervical discectomy and fusion, or ACDF for short.
While there are various methods for doing a cervical fusion, a successful fusion always results in complete loss of motion at the vertebral level being fused.
How Single-Level Fusion Affects Overall Neck Mobility
After the period of 6 to 12 months following ACDF surgery, during which the fusion sets up, a single-level cervical fusion does not significantly affect a patient’s overall cervical range of motion. While motion is lost at the vertebral level that is fused, adjacent levels (one above and below) tend to gain mobility, which mitigates at least some of the loss from the single-level fusion.
See ACDF Surgery Postoperative Care
Furthermore, some patients have even reported more neck mobility compared to before having the single-level fusion.1Hilibrand AS, Balasubramanian K, Eichenbaum M, et al. The effect of anterior cervical fusion on neck motion. Spine. 2006. 31(15):1688-92. This could be due to the fact that prior to having cervical fusion surgery, neck pain has already caused many patients to experience a reduction in active range of motion. If that pain is relieved by the surgery, much of the previously-lost range of motion can be regained.
Also, it should be noted that if a cervical fusion involves one of the top two cervical levels (where the base of the skull—called the occiput—connects to C1 and where C1 connects to C2 below), a significant loss of cervical range of motion will be noticed. Some estimates state that about one-third of the neck’s flexion/extension and half of rotation occurs at these top levels.2Cramer GD. The cervical region. In: Cramer GD, Darby SA, ed. Clinical Anatomy of the Spine, Spinal Cord, and ANS. 3rd ed. St. Louis, MO: Elsevier Mosby; 2013: 135-209. However, it is rare for either of the top levels of the cervical spine to need a fusion.
Does Fusion Lead to Problems at Adjacent Levels?
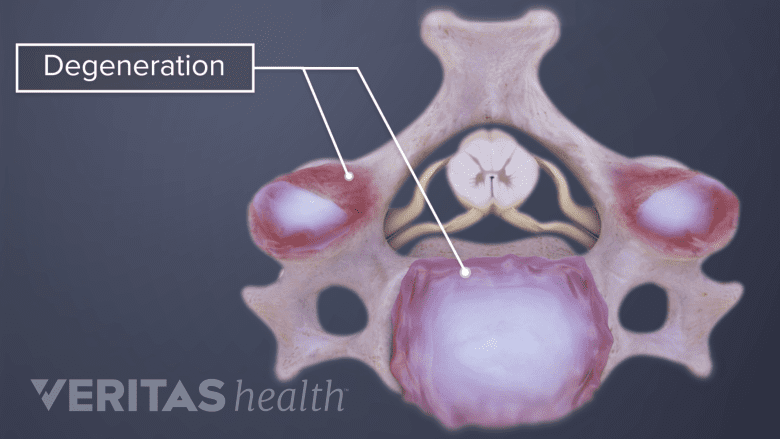
A single-level cervical fusion may cause degeneration in the adjacent levels.
There is some evidence that a single-level cervical fusion could cause adjacent cervical levels to experience more loading stress and thus degenerate sooner, which in some cases could require an additional surgery at a later date. However, not everyone agrees on how much the degeneration might be accelerated and whether it is a significant concern, especially for a single-level fusion.
When a cushioning disc is removed and the spinal level is fused, some of the load previously handled by that joint gets transferred to adjacent joints. The medical literature indicates that more of the load gets transferred to the cervical level beneath the fusion. For example, for C5-C6 fusions, it is more likely for the C6-C7 level to experience more mobility, accelerated degeneration, and possibly an eventual surgery compared to the C4-C5 level.3Anderst WJ, Donaldson WF, Lee JY, Kang JD. Cervical motion segment percent contributions to flexion-extension during continuous functional movement in control subjects and arthrodesis patients. Spine. 2013;38(9):E533-9.
See C5-C6 Treatment and C6-C7 Treatment
Although, it should also be noted that all spinal discs and joints degenerate due to aging over time. If an adjacent level does degenerate, it could be part of the natural history rather than an accelerated occurrence. Also, surgical technique can make a difference. For instance, a wide dissection during surgery may cause injury to an adjacent level and lead to earlier problems at that level than otherwise would have occurred.
See How Cervical Disc Degeneration Occurs
ACDF surgery success rates are relatively high. The need for a reoperation, either at the same or another cervical level, is about 30% within 10 years.4Sasso WR, Smucker JD, Sasso MP, Sasso RC. Long-term Clinical Outcomes of Cervical Disc Arthroplasty: A Prospective, Randomized, Controlled Trial. Spine. 2017;42(4):209-216.
See Anterior Cervical Discectomy and Fusion Complications
For patients who are concerned about a fusion and losing mobility at a cervical level, some could be candidates for cervical artificial disc replacement. Some studies have shown this newer procedure can potentially maintain mobility and reduce stress on adjacent levels.5Fallah A, Akl EA, Ebrahim S, et al. Anterior cervical discectomy with arthroplasty versus arthrodesis for single-level cervical spondylosis: a systematic review and meta-analysis. PLoS ONE. 2012;7(8):e43407.,6Phillips FM, Geisler FH, Gilder KM, Reah C, Howell KM, Mcafee PC. Long-term Outcomes of the US FDA IDE Prospective, Randomized Controlled Clinical Trial Comparing PCM Cervical Disc Arthroplasty With Anterior Cervical Discectomy and Fusion. Spine. 2015;40(10):674-83.
See Artificial Disc Vs. Anterior Cervical Discectomy and Fusion
- 1 Hilibrand AS, Balasubramanian K, Eichenbaum M, et al. The effect of anterior cervical fusion on neck motion. Spine. 2006. 31(15):1688-92.
- 2 Cramer GD. The cervical region. In: Cramer GD, Darby SA, ed. Clinical Anatomy of the Spine, Spinal Cord, and ANS. 3rd ed. St. Louis, MO: Elsevier Mosby; 2013: 135-209.
- 3 Anderst WJ, Donaldson WF, Lee JY, Kang JD. Cervical motion segment percent contributions to flexion-extension during continuous functional movement in control subjects and arthrodesis patients. Spine. 2013;38(9):E533-9.
- 4 Sasso WR, Smucker JD, Sasso MP, Sasso RC. Long-term Clinical Outcomes of Cervical Disc Arthroplasty: A Prospective, Randomized, Controlled Trial. Spine. 2017;42(4):209-216.
- 5 Fallah A, Akl EA, Ebrahim S, et al. Anterior cervical discectomy with arthroplasty versus arthrodesis for single-level cervical spondylosis: a systematic review and meta-analysis. PLoS ONE. 2012;7(8):e43407.
- 6 Phillips FM, Geisler FH, Gilder KM, Reah C, Howell KM, Mcafee PC. Long-term Outcomes of the US FDA IDE Prospective, Randomized Controlled Clinical Trial Comparing PCM Cervical Disc Arthroplasty With Anterior Cervical Discectomy and Fusion. Spine. 2015;40(10):674-83.