The most common risk of a spine fusion surgery is the failure to relieve lower back pain symptoms following the surgery. This outcome is commonly referred to as failed back surgery syndrome.
The likelihood of this result is relatively higher with multilevel fusions involving three or more levels.1Li T, Shi L, Luo Y, Chen D, Chen Y. One-level or multilevel interbody fusion for multilevel lumbar degenerative diseases: a prospective randomized control study with a 4-year follow-up. World Neurosurgery. 2018;110:e815-e822. doi:10.1016/j.wneu.2017.11.109
In This Article:
- Lumbar Spinal Fusion Surgery
- Spine Fusion Risks and Complications
- Lumbar Spinal Fusion Surgery Animation
Procedure-Related Complications in Spinal Fusion
During the surgical procedure itself, several potential complications may occur. These complications can range from minor issues that may be resolved during surgery to more serious complications that require additional interventions.
Infection
Postoperative spine infection can cause increased pain, redness, swelling, or drainage at the surgical site.
The risk factors for infection include2Dowdell J, Brochin R, Kim J, Overley S, Oren J, Freedman B, Cho S. Postoperative Spine Infection: Diagnosis and Management. Global Spine J. 2018 Dec;8(4 Suppl):37S-43S. doi: 10.1177/2192568217745512. Epub 2018 Dec 13. PMID: 30574436; PMCID: PMC6295816.:
- Patient factors, such as age, obesity, and a history of smoking
- Concomitant medical conditions such as malnutrition and diabetes
- Inadequate preparation of the surgical site
Infection places a patient at higher risk for non-fusion (pseudoarthrosis), chronic pain, revision surgery, neurological complications, and delayed recovery.2Dowdell J, Brochin R, Kim J, Overley S, Oren J, Freedman B, Cho S. Postoperative Spine Infection: Diagnosis and Management. Global Spine J. 2018 Dec;8(4 Suppl):37S-43S. doi: 10.1177/2192568217745512. Epub 2018 Dec 13. PMID: 30574436; PMCID: PMC6295816.
Nerve damage
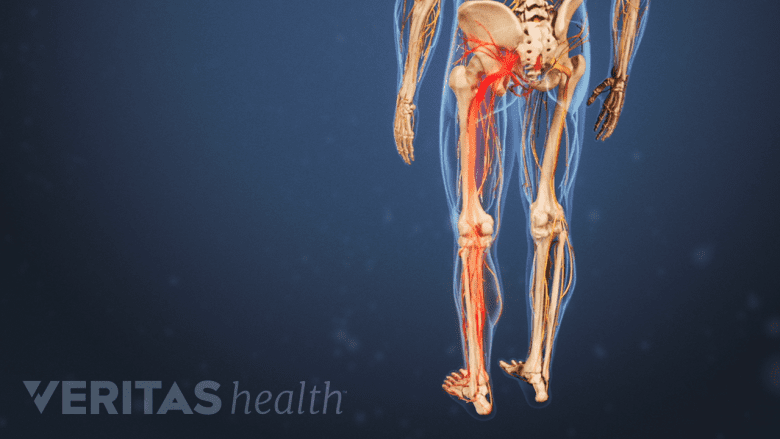
Nerve damage during lumbar spinal fusion surgery may cause leg numbness and weakness.
Nerve damage during a lumbar spinal fusion surgery can result in motor and sensory defects in the low back and legs,3Lykissas MG, Aichmair A, Hughes AP, Sama AA, Lebl DR, Taher F, Du JY, Cammisa FP, Girardi FP. Nerve injury after lateral lumbar interbody fusion: a review of 919 treated levels with identification of risk factors. Spine J. 2014 May 1;14(5):749-58. doi: 10.1016/j.spinee.2013.06.066. Epub 2013 Sep 5. PMID: 24012428. including:
- Pain
- Numbness
- Weakness
- Loss of sensation
Surgical treatment of the lower lumbar levels and longer operating times have been associated with an increased risk of nerve injuries, especially the lumbosacral plexus – a major group of nerves that supply the lower back and legs.3Lykissas MG, Aichmair A, Hughes AP, Sama AA, Lebl DR, Taher F, Du JY, Cammisa FP, Girardi FP. Nerve injury after lateral lumbar interbody fusion: a review of 919 treated levels with identification of risk factors. Spine J. 2014 May 1;14(5):749-58. doi: 10.1016/j.spinee.2013.06.066. Epub 2013 Sep 5. PMID: 24012428.
In some cases, nerve injuries may be temporary and resolve over time, while in others, they may be permanent.
Bleeding
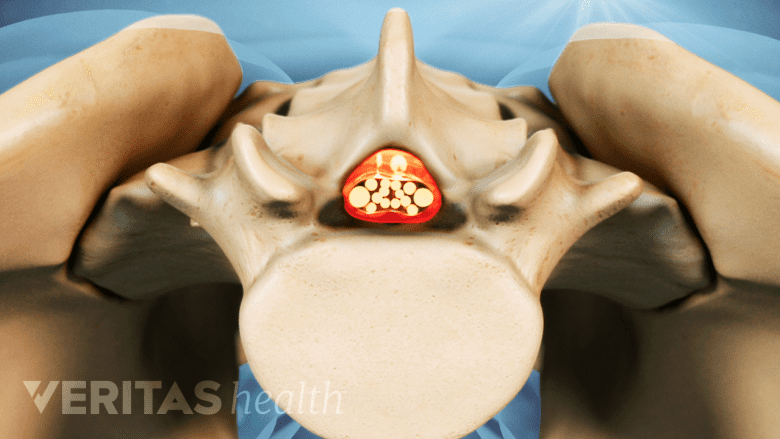
Bleeding during lumbar spinal fusion surgery may be associated with conditions such as spinal canal narrowing.
Bleeding is an inherent risk during any surgical procedure. In a lumbar spinal fusion, a greater risk of bleeding during surgery is associated with4Huang YH, Ou CY. Significant Blood Loss in Lumbar Fusion Surgery for Degenerative Spine. World Neurosurg. 2015 Sep;84(3):780-5. doi: 10.1016/j.wneu.2015.05.007. Epub 2015 May 16. PMID: 25986203.:
- Increase in the number of fused levels
- Severe spinal canal narrowing
Additionally, female sex and low levels of hemoglobin prior to the surgery may increase the risk of blood loss during surgery.4Huang YH, Ou CY. Significant Blood Loss in Lumbar Fusion Surgery for Degenerative Spine. World Neurosurg. 2015 Sep;84(3):780-5. doi: 10.1016/j.wneu.2015.05.007. Epub 2015 May 16. PMID: 25986203.
Intra-operative bleeding can be mitigated by minimally invasive surgical approaches, attention to hemostasis (bleeding control), surgical technique, and hypotensive anesthesia.
Blood transfusions or additional surgical procedures may be necessary to control bleeding and restore circulation.
Complications After Spinal Fusion Surgery
Following spinal fusion surgery, patients may experience postsurgical complications during the recovery period. These complications can vary in severity and duration and may require additional medical attention or interventions.
Potential postsurgical complications include:
Non-union of the fused segments
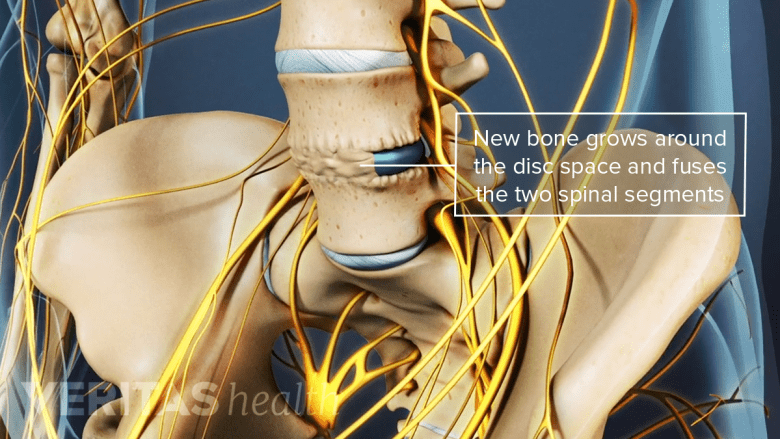
Failure of the spinal segment to heal and fuse into a solid bony segment may lead to spinal instability.
Non-union, or pseudoarthrosis, refers to the failure of the spinal segment to properly heal and fuse into a solid, strong bony segment. Pseudoarthrosis can result in:
- Persistent back pain or radiating pain in the leg and foot
- Spinal instability
- Limited functional improvement
- Increased usage of pain medication5Patel VV, Billys J, Okonkwo DO, He DY, Ryaby JT, Radcliff K. Three- and 4-level lumbar arthrodesis using adjunctive pulsed electromagnetic field stimulation: a multicenter retrospective evaluation of fusion rates and a review of the literature. Int J Spine Surg. 2021;15(2):228-233. doi:10.14444/8031
Fusion failure is a higher risk in the L5-S1 spinal segment.6Tannoury C, Bhale R, Vora M, Saade A, Kortbawi R, Orlando G, Das A, Tannoury T. Pseudarthrosis Following Lumbar and Lumbosacral Fusion Using the Antepsoas Technique. Spine (Phila Pa 1976). 2021 Dec 15;46(24):1690-1695. doi: 10.1097/BRS.0000000000004115. PMID: 34474451.
Implant-related complications
Spinal fusion surgery often involves the use of implants, such as screws, rods, or plates, to stabilize the spine during the healing process. Intra-operative image-guided navigation has improved the accuracy of screw placement by up to 99%.7Shin MH, Ryu KS, Park CK. Accuracy and Safety in Pedicle Screw Placement in the Thoracic and Lumbar Spines : Comparison Study between Conventional C-Arm Fluoroscopy and Navigation Coupled with O-Arm® Guided Methods. J Korean Neurosurg Soc. 2012 Sep;52(3):204-9. doi: 10.3340/jkns.2012.52.3.204. Epub 2012 Sep 30. PMID: 23115662; PMCID: PMC3483320.
See Spine Fusion Instrumentation
Rarely, these implants may break, become loose, or migrate. Revision surgery may be necessary to address these issues and restore spinal stability.
An implant-related problem in the low back is pedicle screw loosening, especially screws placed in the sacrum at level S1. Revision surgery may be needed to fix or remove the hardware.8Zhao Q, Zhang H, Hao D, Guo H, Wang B, He B. Complications of percutaneous pedicle screw fixation in treating thoracolumbar and lumbar fracture. Medicine (Baltimore). 2018;97(29):e11560. doi:10.1097/MD.0000000000011560
Adjacent segment disease
The term ‘adjacent segment disease’ refers to the development of degeneration and instability in the spinal segments adjacent to the fused area. When a spinal motion segment is fused, it becomes immobile, leading to the transfer of stresses to the adjacent spinal motion segments.
Adjacent segment disease may cause:
- Pain
- Reduced mobility
- The need for additional surgeries
In the low back, the fusion of the L4-L5 spinal segment is typically associated with a relatively higher risk of adjacent segment disease.9Lee JC, Choi SW. Adjacent Segment Pathology after Lumbar Spinal Fusion. Asian Spine J. 2015;9(5):807-817. doi:10.4184/asj.2015.9.5.807
It is important to note that radiographic evidence of adjacent segment disease does not always mean that a revision surgery is necessary. Symptomatic adjacent segmental disease is much less common and may require revision surgery.
Strategies to Prevent Postsurgical Complications Following Spinal Fusion
After undergoing spinal fusion surgery, it is crucial to take proactive steps to minimize the risk of complications and ensure a successful recovery. By following the guidelines provided by healthcare professionals and adopting healthy habits, patients can significantly reduce the likelihood of postsurgical complications.
Important measures to help prevent complications after spinal fusion surgery are discussed below.
Follow postsurgical instructions
Carefully adhering to the instructions on resuming activities, adequate wound care, medication guidelines, and physical therapy promotes healing and recovery, lowers the risk of infection, and optimizes the fusion process.
Maintain a healthy lifestyle
Leading a healthy lifestyle plays a significant role in the recovery process.
- Consuming a balanced diet rich in nutrients helps support tissue healing and strengthens bones.
- Staying well-hydrated helps aid in circulation and promotes optimal bodily functions necessary for wound healing.
- Avoiding smoking or any nicotine intake fosters wound healing and the fusion process.
It is advisable to consider quitting smoking or any nicotine intake before surgery and abstain from smoking during the recovery period. Some surgeons also recommend this prior to doing a fusion.
Manage pain and medications
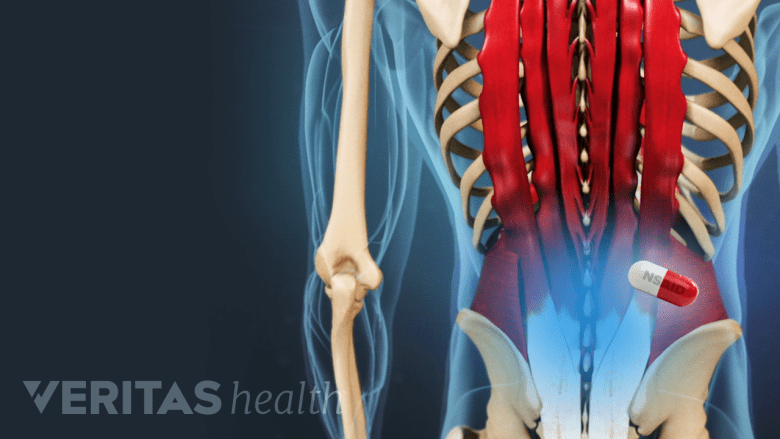
Pain medication helps relieve pain by reducing inflammation and providing a calming effect.
A structured pain management regimen is essential after spinal fusion surgery. Following the prescribed pain medication schedule can help strike a balance between managing pain effectively and avoiding excessive reliance on pain medication.
Overuse of pain medications may lead to complications such as constipation, nausea, and potential addiction. When possible, utilizing alternative pain management techniques, such as ice packs, heat therapy, relaxation techniques, or physical therapy exercises, may help avoid excessive dependence on medication.
Gradually increase activity
Engaging in appropriate physical activity, as guided by the surgeon, is foundational for the recovery process.
Aggressive physical therapy protocols depending on the type of fusion surgery are advised to optimize outcomes. These include spine and core strengthening as well as total body flexibility and strengthening.10Kernc D, Strojnik V, Vengust R. Early initiation of a strength training based rehabilitation after lumbar spine fusion improves core muscle strength: a randomized controlled trial. J Orthop Surg Res. 2018 Jun 19;13(1):151. doi: 10.1186/s13018-018-0853-7. PMID: 29914580; PMCID: PMC6006840. Cardiovascular and endurance training are also important to prevent recurrent injuries.
See Guide to Physical Therapy After Spinal Fusion
Maintain supported posture and body mechanics
Maintaining a well-supported posture and body mechanics is essential to minimize stress on the spine and promote healing.
Supported posture relates to the use of ergonomic principles to ensure proper alignment of the spine and avoid unnecessary strain, such as lifting objects by bending at the knees and leading with the hips rather than bending the back.
Attend follow-up appointments
Regularly attending follow-up appointments with the surgeon and healthcare team allows them to:
- Check progress
- Assess the fusion
- Address any concerns or complications promptly
It is essential to be open and honest during these appointments, discuss any symptoms, and ask concerning questions, which can help the doctor identify potential issues and take immediate action to prevent risks and complications.
Use supportive measures
Using assistive devices like walkers or canes, as recommended by the healthcare provider, can help improve mobility and stability.
The use of a reclining chair and supportive pillows or cushions can help improve comfort and reduce strain on the spine while sitting or sleeping.
It is important to remember that each patient's recovery process may vary. Surgeons provide personalized recommendations based on the specific condition and surgery. By actively participating in the recovery process and closely following medical advice, the risk of postsurgical complications can be reduced and a successful outcome after spinal fusion surgery may be promoted.
- 1 Li T, Shi L, Luo Y, Chen D, Chen Y. One-level or multilevel interbody fusion for multilevel lumbar degenerative diseases: a prospective randomized control study with a 4-year follow-up. World Neurosurgery. 2018;110:e815-e822. doi:10.1016/j.wneu.2017.11.109
- 2 Dowdell J, Brochin R, Kim J, Overley S, Oren J, Freedman B, Cho S. Postoperative Spine Infection: Diagnosis and Management. Global Spine J. 2018 Dec;8(4 Suppl):37S-43S. doi: 10.1177/2192568217745512. Epub 2018 Dec 13. PMID: 30574436; PMCID: PMC6295816.
- 3 Lykissas MG, Aichmair A, Hughes AP, Sama AA, Lebl DR, Taher F, Du JY, Cammisa FP, Girardi FP. Nerve injury after lateral lumbar interbody fusion: a review of 919 treated levels with identification of risk factors. Spine J. 2014 May 1;14(5):749-58. doi: 10.1016/j.spinee.2013.06.066. Epub 2013 Sep 5. PMID: 24012428.
- 4 Huang YH, Ou CY. Significant Blood Loss in Lumbar Fusion Surgery for Degenerative Spine. World Neurosurg. 2015 Sep;84(3):780-5. doi: 10.1016/j.wneu.2015.05.007. Epub 2015 May 16. PMID: 25986203.
- 5 Patel VV, Billys J, Okonkwo DO, He DY, Ryaby JT, Radcliff K. Three- and 4-level lumbar arthrodesis using adjunctive pulsed electromagnetic field stimulation: a multicenter retrospective evaluation of fusion rates and a review of the literature. Int J Spine Surg. 2021;15(2):228-233. doi:10.14444/8031
- 6 Tannoury C, Bhale R, Vora M, Saade A, Kortbawi R, Orlando G, Das A, Tannoury T. Pseudarthrosis Following Lumbar and Lumbosacral Fusion Using the Antepsoas Technique. Spine (Phila Pa 1976). 2021 Dec 15;46(24):1690-1695. doi: 10.1097/BRS.0000000000004115. PMID: 34474451.
- 7 Shin MH, Ryu KS, Park CK. Accuracy and Safety in Pedicle Screw Placement in the Thoracic and Lumbar Spines : Comparison Study between Conventional C-Arm Fluoroscopy and Navigation Coupled with O-Arm® Guided Methods. J Korean Neurosurg Soc. 2012 Sep;52(3):204-9. doi: 10.3340/jkns.2012.52.3.204. Epub 2012 Sep 30. PMID: 23115662; PMCID: PMC3483320.
- 8 Zhao Q, Zhang H, Hao D, Guo H, Wang B, He B. Complications of percutaneous pedicle screw fixation in treating thoracolumbar and lumbar fracture. Medicine (Baltimore). 2018;97(29):e11560. doi:10.1097/MD.0000000000011560
- 9 Lee JC, Choi SW. Adjacent Segment Pathology after Lumbar Spinal Fusion. Asian Spine J. 2015;9(5):807-817. doi:10.4184/asj.2015.9.5.807
- 10 Kernc D, Strojnik V, Vengust R. Early initiation of a strength training based rehabilitation after lumbar spine fusion improves core muscle strength: a randomized controlled trial. J Orthop Surg Res. 2018 Jun 19;13(1):151. doi: 10.1186/s13018-018-0853-7. PMID: 29914580; PMCID: PMC6006840.
Editor’s Top Picks

