Sacroiliac joint fusion surgery may be recommended to treat sacroiliac joint pain when nonsurgical treatments are ineffective.
In a fusion surgery, a bone graft and/or instruments are used to encourage bone growth over the sacroiliac joint and create one immobile unit. Joint fusion can effectively reduce pain and instability caused by sacroiliac joint dysfunction or inflammation (sacroiliitis).
Most cases of sacroiliac joint pain can be treated using pain medication, injection treatments, chiropractic manipulation, and/or physical therapy, and surgery is usually not necessary.
In This Article:
- What to Know About Sacroiliac Joint Fusion
- How Sacroiliac Joint Fusion is Performed
- Sacroiliac Joint Fusion Recovery
Sacroiliac Joint Anatomy and Function

The sacroiliac joint connects the hip bones to the sacrum, primarily acting as a shock absorber.
The sacroiliac joint is a low-motion joint that connects the hip bones to either side of the sacrum, acting primarily as a shock-absorber between the lower body and torso. This joint can also be thought of as the point where the base of the spine connects to the pelvis. The sacroiliac joint is a combination of a synovial joint and the sacroiliac ligaments.
Dysfunction in the sacroiliac joint (also called the SI joint) can produce significant lower back pain, as well as pelvic, groin, and hip pain. Sacroiliac joint dysfunction can be the result of too much motion, too little motion, or inflammation of the joint.
See Sacroiliac Joint Dysfunction Symptoms and Causes
Several studies have found that 15% to 30% of low back pain comes from the sacroiliac joint.1Ledonio CG, Polly DW, Swiontkowski MF. Minimally invasive versus open sacroiliac joint fusion: are they similarly safe and effective?. Clin Orthop Relat Res. 2014;472(6):1831-8. Women who’ve been pregnant have a higher risk for developing SI joint pain due to changes in the pelvis following pregnancy and childbirth. There is compelling evidence that those who have undergone a lumbar spinal fusion are at a heightened risk for SI joint pain.2Cohen SP. Sacroiliac joint pain: a comprehensive review of anatomy, diagnosis, and treatment. Anesth Analg. 2005;101(5):1440-53.
When Is Sacroiliac Joint Fusion an Option?

SI joint fusion is indicated for low back pain with hip or leg stiffness and limited mobility.
When the following symptoms persist for several weeks or months and do not respond to nonsurgical treatment, sacroiliac joint fusion may be recommended:
- Significant low back, hip, or groin pain that makes it difficult to function in everyday life and has not been effectively treated using nonsurgical methods. Sacroiliac joint pain can be felt on one or both sides of the body; one-sided low back pain is an early indication that the SI joint may be the pain generator. Pain is typically confined to the lower back and pelvis, but may radiate down the back of the leg (sciatica).
- Instability in the pelvis and lower back, which may cause pain or difficulty when standing, walking, or moving from sitting to standing or vice versa. Pain may be especially bad when climbing stairs or walking up an incline.
- Stiffness and limited mobility in the low back, hips, groin, or legs.
- Exacerbated pain after sitting or standing for long periods of time, or from certain sleeping positions, such as lying on the affected side for too long.
Sacroiliac joint fusion is always an elective procedure, meaning it is the patient’s decision whether or not to have surgery. There are many factors to consider when deciding to have surgery, including the effectiveness of nonsurgical treatments, if fusion surgery is likely to improve one’s quality of life, and the recovery process necessary after surgery.
Most doctors or back pain specialists will recommend significant trials of nonsurgical methods (at least 8 to 12 weeks, but usually longer) before advising surgery.
Diagnosing SI Joint Pain Before Surgery
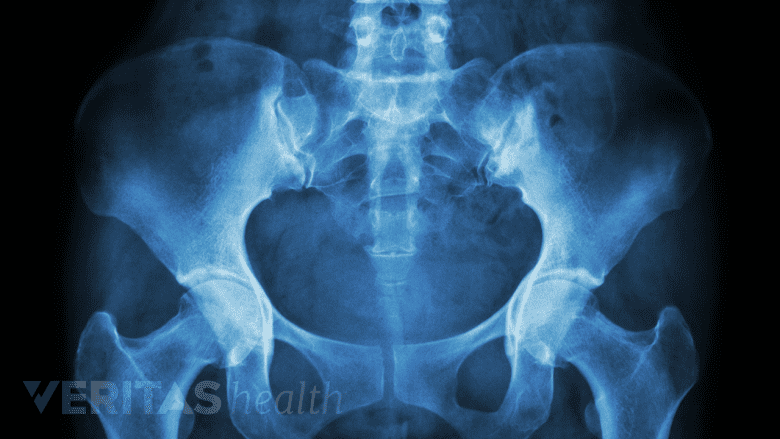
X-rays are helpful in diagnosing sacroiliac joint dysfunction.
Identifying the sacroiliac joint as the primary pain generator can be difficult due to the complex, interconnected nature of the lower spine, pelvis, and hips. For this reason, the diagnostic process for sacroiliac joint pain can be extensive, and typically includes the following process:
- Collected medical history, including information on recent or past injuries that may be causing pain, as well as when pain began and a description of symptoms. A medical history also includes information on sleep habits, exercise and activity, and diet.
- Physical exam, including movement tests designed to provoke or improve symptoms. For example, applying pressure to the sacrum or hips in various directions may cause pain to temporarily alleviate or get worse, indicating that the SI joint is the source of pain. A single movement test is usually inadequate for diagnosis, but a combination of tests can provide an accurate indication of the SI joint as the pain generator.
- Diagnostic imaging tests, including an x-ray, CT, or MRI scan, are mostly used to rule out other possible causes of low back pain. Sacroiliac joint dysfunction does not usually show up well on an imaging test the same way a herniated disc, bone spur, or arthritic joint might. For this reason, an imaging test may not be used at all to diagnose SI joint pain.
- Injection tests are usually the final step in confirming the SI joint as the source of pain. A local anesthetic is injected into the joint space through the low back or buttock. If the injection causes a significant reduction in pain, it indicates that the SI joint is likely the pain generator. Most recommendations suggest a 50% to 75% pain score reduction is needed to confirm the SI joint as the pain source.
See Sacroiliac Joint Injection for Lower Back Pain
It is important that the diagnostic process for SI joint pain and dysfunction consists of multiple methods that inform each other, as there is no single method that has been shown to pinpoint the sacroiliac joint with certainty.2Cohen SP. Sacroiliac joint pain: a comprehensive review of anatomy, diagnosis, and treatment. Anesth Analg. 2005;101(5):1440-53.
- 1 Ledonio CG, Polly DW, Swiontkowski MF. Minimally invasive versus open sacroiliac joint fusion: are they similarly safe and effective?. Clin Orthop Relat Res. 2014;472(6):1831-8.
- 2 Cohen SP. Sacroiliac joint pain: a comprehensive review of anatomy, diagnosis, and treatment. Anesth Analg. 2005;101(5):1440-53.
Editor’s Top Picks

