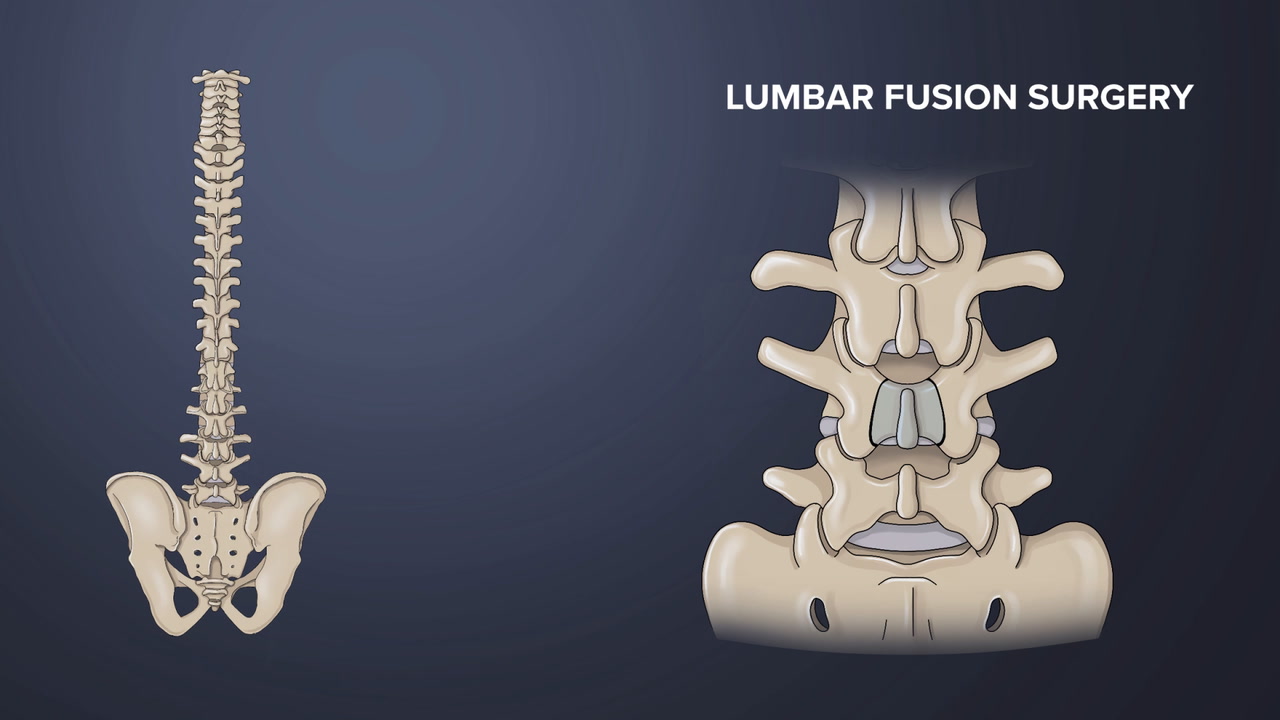
TLIF is a type of spinal fusion surgery designed to create solid bone and eliminate motion in a spinal segment. Lumbar fusion surgery may be recommended to alleviate ongoing, disabling pain caused by conditions such as spondylolisthesis, degenerative disc disease, and/or recurrent disc herniations.
In This Article:
- Transforaminal Lumbar Interbody Fusion (TLIF) Back Surgery
- TLIF Back Surgery Success Rates and Risks
Understanding TLIF (Transforaminal Lumbar Interbody Fusion) Procedure for Spinal Fusion
The transforaminal space is a small opening between adjacent vertebrae.
The abbreviation TLIF stands for:
- Transforaminal refers to the surgical approach through the hollow bony openings (foramina) between adjacent spinal segments
- Lumbar, referring to the lumbar spine in the lower back
- Interbody, meaning the area between two adjacent vertebral bones in the spine
- Fusion refers to the process of two bones becoming one
TLIF fuses the anterior (front) and posterior (back) columns of the spine through a single posterior approach. This article describes the TLIF technique and compares TLIF to other approaches to spinal fusion.
TLIF Indications and Contraindications
Chronic spondylolisthesis pain may sometimes be treated with TLIF surgery.
Lumbar spine fusion may be recommended for disabling low back and/or leg symptoms that have not improved with nonsurgical forms of treatment.
TLIF may be indicated when back and/or leg pain is due to1Mobbs RJ, Phan K, Malham G, Seex K, Rao PJ. Lumbar interbody fusion: techniques, indications and comparison of interbody fusion options including PLIF, TLIF, MI-TLIF, OLIF/ATP, LLIF and ALIF. J Spine Surg. 2015;1(1):2-18. doi:10.3978/j.issn.2414-469X.2015.10.05:
- Spondylolisthesis, the slipping of one vertebral body over another
- Degenerative disc disease with foraminal stenosis, resulting in nerve compression
- Recurrent disc herniations, which occur when the inner material of the disc leaks into the disc’s weakened outer layer
- Pseudoarthrosis, the lack of a solid fusion from a prior fusion surgery
TLIF may be the preferred approach (over posterior lumbar interbody fusion) when disc degeneration is predominantly one-sided—and depends on the surgeon’s expertise.2Fleege C, Rickert M, Rauschmann M. PLIF- und TLIF-Verfahren. Indikation, Technik, Vor- und Nachteile [The PLIF and TLIF techniques. Indication, technique, advantages, and disadvantages]. Orthopade. 2015;44(2):114-123. doi:10.1007/s00132-014-3065-9
Contraindications for TLIF include active neurological issues and/or weakened bone, such as in1Mobbs RJ, Phan K, Malham G, Seex K, Rao PJ. Lumbar interbody fusion: techniques, indications and comparison of interbody fusion options including PLIF, TLIF, MI-TLIF, OLIF/ATP, LLIF and ALIF. J Spine Surg. 2015;1(1):2-18. doi:10.3978/j.issn.2414-469X.2015.10.05:
- Extensive epidural scarring
- Arachnoiditis (inflammation in the spinal canal)
- Active infection
- Conjoined nerve roots
- Osteoporosis
General contraindications of any spinal fusion procedure, such as excessive thinning of spinal bones due to osteoporosis, and conditions that act as an obstacle to accessing the disc space, may also make TLIF an unfavorable option.
Procedure for Spine Fusion Using TLIF Technique
In TLIF surgery, a vertical incision is made along the midline of the back.
Prior to any form of lumbar spine fusion, medical clearance is obtained and patients who smoke are required to stop. Patients may donate their own blood, if they choose, to be used at the time of surgery.
TLIF surgery fuses the anterior (front) and posterior (back) columns of the spine through a single posterior approach. Surgical hardware is applied to the spine to help enhance the fusion rate. The anterior portion of the spine is stabilized by the bone graft and interbody spacer. The posterior column is locked in place with pedicle screws, rods, and bone graft. As the bone graft heals, it fuses the vertebra above and below and forms one long bone.
More specifically, a step-by-step approach to the TLIF surgical procedure involves1Mobbs RJ, Phan K, Malham G, Seex K, Rao PJ. Lumbar interbody fusion: techniques, indications and comparison of interbody fusion options including PLIF, TLIF, MI-TLIF, OLIF/ATP, LLIF and ALIF. J Spine Surg. 2015;1(1):2-18. doi:10.3978/j.issn.2414-469X.2015.10.05,3Gum JL, Reddy D, Glassman S. Transforaminal Lumbar Interbody Fusion (TLIF). JBJS Essent Surg Tech. 2016;6(2):e22. Published 2016 Jun 8. doi:10.2106/JBJS.ST.15.00003:
- Preparing the patient. The patient receives general anesthesia and is positioned face-down on the operating table. The surgical site is prepared with antiseptic solution and local anesthesia.
- Accessing the spine. In a unilateral (one-sided) approach during open TLIF, a single vertical incision between 2 to 4 inches long is made along the midline of the back at the level of the affected intervertebral disc. In a bilateral (two-sided) approach during minimally invasive TLIF, two small incisions are made on either side of the midline of the back. In both approaches, the surgeon cuts through layers of fat and muscle and retracts them to the side.
- Placing the screws. Screws are placed for supplemental posterior fixation to enhance the stability of the spinal segment being treated. The screws are named after their placement; for example, pedicle screws are placed into the pedicle located in the back of the vertebra.
- Exposing the disc space. The disc space is located in the front of the spine, between two vertebral bodies. During surgery, this disc space is accessed by drilling from one side and removing the lamina and/or the facet joint. Approaching the disc space using this technique allows access to the damaged disc and the subsequent delivery of bone graft material with minimal retraction of important nerves—the thecal sac and nerve roots.
- Replacing the disc with a bone graft. After gaining access to the disc, the disc material is removed. The surgeon then places an interbody spacer or interbody cage that is filled with a bone graft. The spacer or cage is put into place from one side of the spine. If a posterolateral fusion is performed alongside the TLIF, then additional bone graft material may be placed in the lateral (side) gutters of the vertebra and the disc space.
- Using an interbody spacer. A static or expandable spacer4Kremer MA, Alferink J, Wynsma S, Shirk T, Ledonio C. Expandable spacers provide better functional outcomes than static spacers in minimally invasive transforaminal lumbar interbody fusion. J Spine Surg. 2019;5(3):315-319. doi:10.21037/jss.2019.06.07 can be inserted into the disc space, helping to restore normal disc height and opening up the nerve foramina to take pressure off the nerve roots. By restoring the disc height of the fused segments during TLIF, the spacer can help re-create normal spinal alignment.
- Completing the fixation of the vertebrae. Pedicle screws are attached to rods or plates. These screw-rod constructs stabilize the vertebral segments of the spine, holding the motion segment in place and allowing the bone graft to fuse the segments into one bone over time. X-rays may be taken during the surgery to ensure the correct placement of hardware.
- Closing the wound. After the surgery is completed, the wound is closed with dissolving sutures (stitches). Careful attention is given to avoid wound complications and infections, which are well-known risks following spine surgery.
TLIF can be performed as an open surgery or a minimally invasive surgery, which involves a smaller incision and specialized tools.
Watch Lumbar Spinal Fusion Surgery Animation
Post-surgical Care After TLIF
After a standard TLIF spinal fusion surgery, patients are admitted to the hospital for an average of 2 to 4 days. During the post-surgical period, patients may:
- Be closely monitored for any signs of infection, such as fever
- Experience pain at the incision site, which is usually managed using oral pain medications
- Undergo a computed tomographic (CT) scan, which is performed the day after surgery
- Receive physical therapy, which typically begins the day after surgery to improve mobility and avoid blood clots
- Use a spinal brace up to 3 months after surgery, which may help the recovery process
Patients are discharged with recommendations to limit activity. While light walking is recommended, the most essential cautions during recovery are to avoid lifting heavy objects, bending or twisting the back, or sitting continuously for long periods of time. Any feeling of tingling or numbness in the leg(s) must be reported to the surgeon.
Generally, patients can return to work in 4 to 6 weeks, or longer, if the patient’s occupation is more physically demanding. A follow-up with the surgeon is typically scheduled for a date several weeks after surgery.
Advantages of TLIF over other forms of lumbar fusion may include:
- Direct neurologic decompression. The TLIF approach allows direct access to the nerves and a thorough neurologic decompression. Compared to approaches such as anterior lumbar interbody fusion (ALIF) and extreme lumbar interbody fusion (XLIF), the surgeon does not rely on "indirect" decompression to achieve pain relief.
- Single approach/single position procedure. Compared to other techniques for spinal fusion surgery such as ALIF or XLIF, which require two separate incisions in two different positions, the TLIF procedure is done through a single posterior approach, which can often result in less time in surgery and under anesthesia.
- Foraminal height restoration. Compared to a traditional posterolateral fusion, a TLIF approach allows for the re-establishment of disc height, and in turn, restoration of foraminal height, which can help with neurologic decompression.
The benefits of TLIF come alongside certain disadvantages to the approach, such as difficulty in extensive preparation of the endplates for cage insertion or difficulty in restoring lordosis, the spine’s natural curvature.
TLIF is a more recent approach to spinal fusion and approaches the disc space through the bony openings or foramen that allow nerves to exit the spine. While available research on TLIF is limited, the procedure remains promising and offers important advantages that may enhance long-term outcomes after surgery.
- 1 Mobbs RJ, Phan K, Malham G, Seex K, Rao PJ. Lumbar interbody fusion: techniques, indications and comparison of interbody fusion options including PLIF, TLIF, MI-TLIF, OLIF/ATP, LLIF and ALIF. J Spine Surg. 2015;1(1):2-18. doi:10.3978/j.issn.2414-469X.2015.10.05
- 2 Fleege C, Rickert M, Rauschmann M. PLIF- und TLIF-Verfahren. Indikation, Technik, Vor- und Nachteile [The PLIF and TLIF techniques. Indication, technique, advantages, and disadvantages]. Orthopade. 2015;44(2):114-123. doi:10.1007/s00132-014-3065-9
- 3 Gum JL, Reddy D, Glassman S. Transforaminal Lumbar Interbody Fusion (TLIF). JBJS Essent Surg Tech. 2016;6(2):e22. Published 2016 Jun 8. doi:10.2106/JBJS.ST.15.00003
- 4 Kremer MA, Alferink J, Wynsma S, Shirk T, Ledonio C. Expandable spacers provide better functional outcomes than static spacers in minimally invasive transforaminal lumbar interbody fusion. J Spine Surg. 2019;5(3):315-319. doi:10.21037/jss.2019.06.07