Physical therapy and exercise are essential components of a treatment plan for sacroiliac (SI) joint dysfunction pain relief and recovery.
In This Article:
Effectiveness of Exercise and Physical Therapy in Relieving SI Joint Pain
Physical therapy may help control pain originating from the SI joint.
The sacroiliac joint, which connects the spine to the hip, can cause pain in the buttock, groin, back of the thigh, and/or lower part of the leg due to abnormal motion at the joint.1Barros G, McGrath L, Gelfenbeyn M. Sacroiliac Joint Dysfunction in Patients With Low Back Pain. Fed Pract. 2019;36(8):370-375.
An estimated 15% to 30% of low back pain cases originate at the sacroiliac joint.2Buchanan BK, Varacallo M. Sacroiliitis. [Updated 2022 Sep 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK448141/ Research indicates that most patients respond well to physical therapy and exercise to manage their symptoms and prevent the progression of the condition.1Barros G, McGrath L, Gelfenbeyn M. Sacroiliac Joint Dysfunction in Patients With Low Back Pain. Fed Pract. 2019;36(8):370-375.,3Al-Subahi M, Alayat M, Alshehri MA, et al. The effectiveness of physiotherapy interventions for sacroiliac joint dysfunction: a systematic review. J Phys Ther Sci. 2017;29(9):1689-1694. http://doi.org/10.1589/jpts.29.1689
How Therapeutic Exercise Helps Manage SI Joint Pain
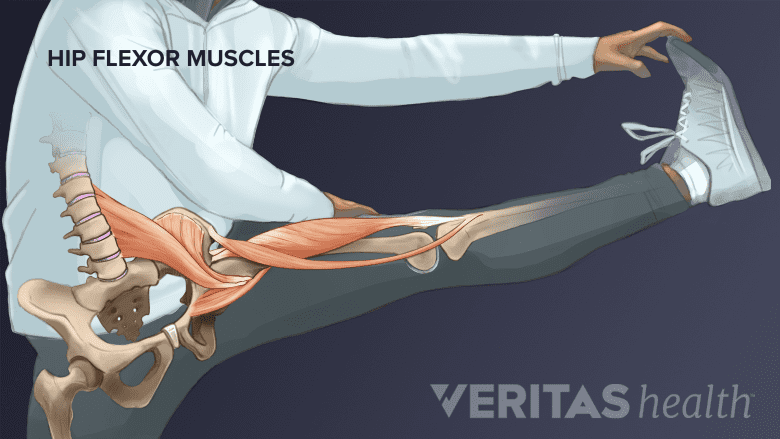
SI joint exercises target the lower back and leg muscles.
Exercise therapy for SI joint pain relief consists of a series of guided stretching and strengthening exercises that aim to restore natural movement in the joint, by:
- Relaxing tense muscles and ligaments that limit natural motion within the joint
- Conditioning the surrounding muscles and strengthening the ligaments to better support the joint
Exercises target several muscle groups in the abdomen and lower limbs.
5 Essential Treatment Aspects of a Physical Therapy Program for SI Joint Pain
As one of the first-line treatments, guided physical therapy for SI joint pain relief aims to provide long-term improvement and symptom control through a set of 5 treatment aspects described below:
-
Educating the patient
Patient education involves guidance on exercises and lifestyle modifications to reduce symptom recurrence.
- Patient education is a critical component of a physical therapy treatment plan. Physical therapists provide guidance on proper body mechanics, posture, and lifestyle modifications that may help reduce or prevent the recurrence of SI joint pain.3Al-Subahi M, Alayat M, Alshehri MA, et al. The effectiveness of physiotherapy interventions for sacroiliac joint dysfunction: a systematic review. J Phys Ther Sci. 2017;29(9):1689-1694. http://doi.org/10.1589/jpts.29.1689
- By understanding how to move their bodies safely and effectively, patients can speed up their recovery and prevent re-injury. Patient education is also important for chronic pain patients, as it can help them manage their symptoms and maintain their independence.
-
Controlling inflammation and pain
Heat and cold therapy can help effectively control SI joint inflammation.
- Inflammation and pain are closely related and can cause significant discomfort, reducing the quality of life. Therapeutic treatments that may help reduce inflammation, pain, and discomfort include3Al-Subahi M, Alayat M, Alshehri MA, et al. The effectiveness of physiotherapy interventions for sacroiliac joint dysfunction: a systematic review. J Phys Ther Sci. 2017;29(9):1689-1694. http://doi.org/10.1589/jpts.29.1689:
-
- Manual therapy, which involves hands-on techniques to mobilize soft tissue and modulate pain.4Ulger O, Demirel A, Oz M, Tamer S. The effect of manual therapy and exercise in patients with chronic low back pain: Double blind randomized controlled trial. Journal of Back and Musculoskeletal Rehabilitation. 2017;30(6):1303-1309. http://doi.org/10.3233/BMR-169673 This therapy can help relieve stiffness and increase the range of motion in the joint, potentially reducing pain and inflammation and promoting muscle relaxation.4Ulger O, Demirel A, Oz M, Tamer S. The effect of manual therapy and exercise in patients with chronic low back pain: Double blind randomized controlled trial. Journal of Back and Musculoskeletal Rehabilitation. 2017;30(6):1303-1309. http://doi.org/10.3233/BMR-169673
- Massage therapy, which involves manipulating the soft tissues in the body, including muscles, tendons, and ligaments, to reduce pain and inflammation. Therapeutic massages can help improve circulation, increase flexibility, and reduce stress—all of which can contribute to reducing inflammation and pain.5Salvo SG. Massage Therapy: Principles and Practice. 5th ed. Elsevier; 2016.
- Ultrasound therapy, a non-invasive treatment that uses high-frequency sound waves to stimulate tissue healing and reduce inflammation in deep musculoskeletal tissues. This therapy aims to increase blood flow, extensibility of the connective tissues, and tissue regeneration – thereby promoting healing.6Ebadi S, Henschke N, Forogh B, et al. Therapeutic ultrasound for chronic low back pain. Cochrane Database Syst Rev. 2020;7(7):CD009169. http://doi.org/10.1002/14651858.CD009169.pub3 Research indicates that ultrasound therapy provides limited benefits and may only be used for short-term treatments.
- Transcutaneous electric nerve stimulation (TENS), a therapy that uses low-voltage electric currents to stimulate the nerves and reduce pain. TENS therapy works by sending electrical impulses through the skin to the affected area, which in turn helps block pain signals from reaching the brain.7Seco J, Kovacs FM, Urrutia G. The efficacy, safety, effectiveness, and cost-effectiveness of ultrasound and shock wave therapies for low back pain: a systematic review. The Spine Journal. 2011;11(10):966-977. https://doi.org/10.1016/j.spinee.2011.02.002
- Heat therapy, a treatment that helps reduce pain by increasing blood flow, relaxing muscles, and reducing stiffness.8Petrofsky J, Paluso D, Anderson D, et al. The contribution of skin blood flow in warming the skin after the application of local heat; the duality of the Pennes heat equation. Med Eng Phys. 2011;33(3):325-329. http://doi.org/10.1016/j.medengphy.2010.10.018
- Ice therapy, a treatment to reduce pain and swelling in the affected area.
- To avoid injury, heat/ice should not be applied directly to the skin, and application time should be limited to 10 to 20 minutes with two-hour breaks in between applications.
Improving flexibility
Improving flexibility can improve athletic performance and reduce the risk of injury.
- Once the inflammation and pain are under control, the physical therapist focuses on improving flexibility through guided techniques and flexibility exercises to perform at home.
- Flexibility exercises can help to maintain joint mobility, reduce muscle tension, improve posture, increase range of motion, and reduce the risk of injury. Increased flexibility can also improve athletic performance and help reduce muscle soreness and fatigue.9Behm DG, Chaouachi A. A review of the acute effects of static and dynamic stretching on performance. Eur J Appl Physiol . 2011;11:2633-2651. https://doi.org/10.1007/s00421-011-1879-2
Increasing strength
SI joint strengthening exercises target the lower back, buttocks, hip, and hamstring muscles.
- Strengthening the muscle groups in the lower back, abdomen, pelvis, and thigh helps improve stability, balance, and function in the lower back, pelvis, and legs.
- Guidelines for therapeutic exercises for SI joint pain focus on mobilizing the pelvic and hip joints and stabilizing the spine through core-strengthening exercises.10Nejati P, Safarcherati A, Karimi F. Effectiveness of exercise therapy and manipulation on sacroiliac joint dysfunction: a randomized controlled trial. Pain Physician. 2019;22(1):53-61. The key to an effective exercise program for SI joint health is to work on strengthening the contralateral muscles (muscles on the opposite side of the body) in the back, buttocks, and legs at the same time.11Vleeming A, Schuenke MD, Masi AT, Carreiro JE, Danneels L, Willard FH. The sacroiliac joint: an overview of its anatomy, function and potential clinical implications. J Anat. 2012;221(6):537-567. http://doi.org/10.1111/j.1469-7580.2012.01564.x,12Falowski S, Sayed D, Pope J, et al. A Review and Algorithm in the Diagnosis and Treatment of Sacroiliac Joint Pain. Journal of Pain Research. 2020;13:3337-3348.
- Specifically, the following groups of muscles are targeted in an SI joint exercise program:
- Buttock muscles, including the gluteus maximus13Added MAN, de Freitas DG, Kasawara KT, Martin RL, Fukuda TY. STRENGTHENING THE GLUTEUS MAXIMUS IN SUBJECTS WITH SACROILIAC DYSFUNCTION. Int J Sports Phys Ther. 2018;13(1):114-120. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5808006/ and gluteus medius14Yoo WG. Effects of individual strengthening exercises on subdivisions of the gluteus medius in a patient with sacroiliac joint pain. J Phys Ther Sci. 2014;26(9):1501-1502. http://doi.org/10.1589/jpts.26.1501
- Back muscles, including the erector spinae15Yoo WG. Effects of individual strengthening exercises for the stabilization muscles on the nutation torque of the sacroiliac joint in a sedentary worker with nonspecific sacroiliac joint pain. J Phys Ther Sci. 2015;27(1):313-314. http://doi.org/10.1589/jpts.27.313
- Abdominal muscles, such as the rectus abdominis8Petrofsky J, Paluso D, Anderson D, et al. The contribution of skin blood flow in warming the skin after the application of local heat; the duality of the Pennes heat equation. Med Eng Phys. 2011;33(3):325-329. http://doi.org/10.1016/j.medengphy.2010.10.018
- Hamstrings9Behm DG, Chaouachi A. A review of the acute effects of static and dynamic stretching on performance. Eur J Appl Physiol . 2011;11:2633-2651. https://doi.org/10.1007/s00421-011-1879-2
- These muscle groups play an essential role in supporting the body's weight and movement during activities such as walking, running, and standing.
Developing endurance
Aerobic exercises can build muscle endurance and increase stamina.
- The final step of a physical therapy program is to develop endurance in the muscle groups to help maintain muscle balance even when the region is fatigued.
- Engaging in aerobic exercises, such as walking, low-impact cardiovascular exercise, or swimming, are common ways to develop muscle endurance and increase stamina. When engaging in aerobic exercises, it is essential to avoid activities that involve spreading the legs too far front, back, or side to side in an asymmetrical manner, to minimize discomfort on the SI joint.
See Common Triggers of SI Joint Pain and How to Prevent a Flare-up
It is recommended that a doctor or physical therapist familiar with the patient’s specific needs is consulted before starting a new exercise program. A prior consultation ensures that a new exercise will not cause further exacerbation of pain.
Understanding SI Joint Mobility: Hypermobility vs Hypomobility and the Impact on Physical Therapy
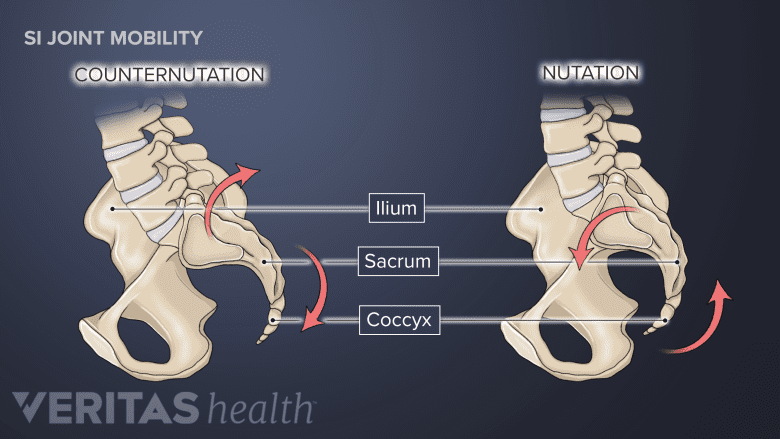
A normal SI joint can move forward and downward (nutation) and backward and upward (counternutation).
Understanding what the body needs is a crucial step toward an effective physical therapy program for the SI joint. Pain in this joint typically occurs due to hypermobility or hypomobility of the joint.16Dydyk AM, Forro SD, Hanna A. Sacroiliac Joint Injury. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2022. https://pubmed.ncbi.nlm.nih.gov/32491804/
Hypermobility of the SI joint means that the joint moves more than the normal limit, while hypomobility of the SI joint means that the joint doesn’t move enough.16Dydyk AM, Forro SD, Hanna A. Sacroiliac Joint Injury. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2022. https://pubmed.ncbi.nlm.nih.gov/32491804/ Both mechanisms can lead to discomfort and pain in the SI joint and surrounding areas, and the treatment approach varies for the specific underlying cause.
Common causes for SI joint dysfunction are traumatic or jarring events that involve one leg or one side of the pelvis. A few examples include stepping off a step thinking there is another below it, stepping into a hole while walking or jogging, or a rear-end accident with the right foot depressing the brake/twisting the pelvis.
Managing SI joint hypermobility with physical therapy and exercise
Traumatic injuries, such as falls, can result in hypermobility of the SI joint.
Hypermobility of the SI joint often results from ligaments in the joint becoming loose, typically due to injury or pregnancy, making the joint more mobile than usual.16Dydyk AM, Forro SD, Hanna A. Sacroiliac Joint Injury. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2022. https://pubmed.ncbi.nlm.nih.gov/32491804/,17Newman DP, Soto A. Sacroiliac Joint Dysfuction: Diagnosis and Treatment. Am Fam Physician. 2022;105(3):239-245. https://pubmed.ncbi.nlm.nih.gov/35289578/ Over time, this excessive movement can cause inflammation and pain in the joint.
To manage a hypermobile SI joint, physical therapists focus on strengthening the muscles around the SI joint, including the abdominals, buttocks, and lower back muscles.16Dydyk AM, Forro SD, Hanna A. Sacroiliac Joint Injury. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2022. https://pubmed.ncbi.nlm.nih.gov/32491804/ These exercises help stabilize the joint, reducing excessive movement and associated pain.
Managing SI joint hypomobility with physical therapy and exercise
Arthritis is a common cause of hypomobility of the SI joint.
Hypomobility of the SI joint is typically a result of aging, arthritis, or previous surgery in the area that leads to scar tissue formation.16Dydyk AM, Forro SD, Hanna A. Sacroiliac Joint Injury. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2022. https://pubmed.ncbi.nlm.nih.gov/32491804/ The stiffness and restricted movement in the joint can cause a dull ache or sharp pain in the lower back or buttocks.
To manage a hypomobile SI joint, manipulation therapy and appropriate stretching and strengthening exercises are recommended. Stretching exercises increase flexibility, improve range of motion, and enhance overall joint function.18Lee J, Yoo W. Application of posterior pelvic tilt taping for the treatment of chronic low back pain with sacroiliac joint dysfunction and increased sacral horizontal angle. Physical Therapy in Sport. 2012;13(4):279-285. https://doi.org/10.1016/j.ptsp.2011.10.003 Specific stretches targeting the lower back, buttocks, and hip areas may benefit patients with hypomobile SI joints.19Shokri E, Kamali F, Sinaei E, Ghafarinejad F. Spinal manipulation in the treatment of patients with MRI-confirmed lumbar disc herniation and sacroiliac joint hypomobility: a quasi-experimental study. Chiropractic & Manual Therapies. 2018; 26(16). https://doi.org/10.1186/s12998-018-0185-z
Duration of a Guided Physical Therapy and Exercise Program for SI Joint Pain
The guidelines for treating sacroiliac joint dysfunction are usually similar to treating most other musculoskeletal problems. The total length of an exercise program depends on the severity and duration of the symptoms and signs.
Exercise and physical therapy typically start with a few sessions performed under the guidance of a therapist followed by a longer-term home program. If the pain and other symptoms resolve, no further visits are needed, and the home exercises may be continued.
- 1 Barros G, McGrath L, Gelfenbeyn M. Sacroiliac Joint Dysfunction in Patients With Low Back Pain. Fed Pract. 2019;36(8):370-375.
- 2 Buchanan BK, Varacallo M. Sacroiliitis. [Updated 2022 Sep 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK448141/
- 3 Al-Subahi M, Alayat M, Alshehri MA, et al. The effectiveness of physiotherapy interventions for sacroiliac joint dysfunction: a systematic review. J Phys Ther Sci. 2017;29(9):1689-1694. http://doi.org/10.1589/jpts.29.1689
- 4 Ulger O, Demirel A, Oz M, Tamer S. The effect of manual therapy and exercise in patients with chronic low back pain: Double blind randomized controlled trial. Journal of Back and Musculoskeletal Rehabilitation. 2017;30(6):1303-1309. http://doi.org/10.3233/BMR-169673
- 5 Salvo SG. Massage Therapy: Principles and Practice. 5th ed. Elsevier; 2016.
- 6 Ebadi S, Henschke N, Forogh B, et al. Therapeutic ultrasound for chronic low back pain. Cochrane Database Syst Rev. 2020;7(7):CD009169. http://doi.org/10.1002/14651858.CD009169.pub3
- 7 Seco J, Kovacs FM, Urrutia G. The efficacy, safety, effectiveness, and cost-effectiveness of ultrasound and shock wave therapies for low back pain: a systematic review. The Spine Journal. 2011;11(10):966-977. https://doi.org/10.1016/j.spinee.2011.02.002
- 8 Petrofsky J, Paluso D, Anderson D, et al. The contribution of skin blood flow in warming the skin after the application of local heat; the duality of the Pennes heat equation. Med Eng Phys. 2011;33(3):325-329. http://doi.org/10.1016/j.medengphy.2010.10.018
- 9 Behm DG, Chaouachi A. A review of the acute effects of static and dynamic stretching on performance. Eur J Appl Physiol . 2011;11:2633-2651. https://doi.org/10.1007/s00421-011-1879-2
- 10 Nejati P, Safarcherati A, Karimi F. Effectiveness of exercise therapy and manipulation on sacroiliac joint dysfunction: a randomized controlled trial. Pain Physician. 2019;22(1):53-61.
- 11 Vleeming A, Schuenke MD, Masi AT, Carreiro JE, Danneels L, Willard FH. The sacroiliac joint: an overview of its anatomy, function and potential clinical implications. J Anat. 2012;221(6):537-567. http://doi.org/10.1111/j.1469-7580.2012.01564.x
- 12 Falowski S, Sayed D, Pope J, et al. A Review and Algorithm in the Diagnosis and Treatment of Sacroiliac Joint Pain. Journal of Pain Research. 2020;13:3337-3348.
- 13 Added MAN, de Freitas DG, Kasawara KT, Martin RL, Fukuda TY. STRENGTHENING THE GLUTEUS MAXIMUS IN SUBJECTS WITH SACROILIAC DYSFUNCTION. Int J Sports Phys Ther. 2018;13(1):114-120. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5808006/
- 14 Yoo WG. Effects of individual strengthening exercises on subdivisions of the gluteus medius in a patient with sacroiliac joint pain. J Phys Ther Sci. 2014;26(9):1501-1502. http://doi.org/10.1589/jpts.26.1501
- 15 Yoo WG. Effects of individual strengthening exercises for the stabilization muscles on the nutation torque of the sacroiliac joint in a sedentary worker with nonspecific sacroiliac joint pain. J Phys Ther Sci. 2015;27(1):313-314. http://doi.org/10.1589/jpts.27.313
- 16 Dydyk AM, Forro SD, Hanna A. Sacroiliac Joint Injury. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2022. https://pubmed.ncbi.nlm.nih.gov/32491804/
- 17 Newman DP, Soto A. Sacroiliac Joint Dysfuction: Diagnosis and Treatment. Am Fam Physician. 2022;105(3):239-245. https://pubmed.ncbi.nlm.nih.gov/35289578/
- 18 Lee J, Yoo W. Application of posterior pelvic tilt taping for the treatment of chronic low back pain with sacroiliac joint dysfunction and increased sacral horizontal angle. Physical Therapy in Sport. 2012;13(4):279-285. https://doi.org/10.1016/j.ptsp.2011.10.003
- 19 Shokri E, Kamali F, Sinaei E, Ghafarinejad F. Spinal manipulation in the treatment of patients with MRI-confirmed lumbar disc herniation and sacroiliac joint hypomobility: a quasi-experimental study. Chiropractic & Manual Therapies. 2018; 26(16). https://doi.org/10.1186/s12998-018-0185-z