The cervical spine plays key roles in supporting the head’s weight and mobility, as well as facilitating electrical signals and blood flow between the brain and the rest of the body. Consisting of seven vertebrae and six intervertebral discs, muscles, tendons, ligaments, blood vessels, and nerves, the cervical spine is a complex structure.
In This Article:
Natural History of the Cervical Spine

The adult cervical spine balances the head, protects the spinal cord, and provides mobility to the neck.
A typical cervical spine goes through the following lifecycle.
- Birth to age 2. At birth, the cervical discs are large and round, filled with cushioning liquid gel. The comparatively small vertebral bodies start out almost spherical in shape, similar to a watermelon. At about 3 months, the cervical lordosis (backward curve of the neck) develops as the baby starts lifting his or her head. During these first few years, the head is wobbly due to the relatively small cervical spine and the developing postural muscles and ligaments that hold it up. The cervical spine’s most mobile segment is initially located at the C2-C3 vertebral level.1Cramer GD, Y SW. Unique anatomic features of the pediatric spine. In: Cramer GD, Darby SA, ed. Clinical Anatomy of the Spine, Spinal Cord, and ANS. 3rd ed. St. Louis, MO: Elsevier Mosby; 2014: 566-85.
- Ages 2 to 10. The cervical discs start to flatten out and assume a less rounded shape while the vertebral bodies become comparatively larger and more rectangular. The cervical lordosis curve tends to become larger until age 5 and then becomes less pronounced as the cervical vertebrae continue to change shape and postural muscles and ligaments start to better support the head.1Cramer GD, Y SW. Unique anatomic features of the pediatric spine. In: Cramer GD, Darby SA, ed. Clinical Anatomy of the Spine, Spinal Cord, and ANS. 3rd ed. St. Louis, MO: Elsevier Mosby; 2014: 566-85.
- Adolescence. By early adolescence, the cervical spine has mostly taken its adult shape, although its size will continue to grow for a few more years. Compared to the younger cervical spine, the adolescent spine has less space for nerve roots to exit through the spinal canal’s bony holes, called foramina. This change arises because facet joints, in the back (posterior) portion of the cervical spine, angle downward more and have developed more bone while the nerve root has also gotten bigger. The most mobile segment of the cervical spine has now moved from C2-C3 all the way down to C5-C6 where it remains through the rest of adolescence and adulthood.1Cramer GD, Y SW. Unique anatomic features of the pediatric spine. In: Cramer GD, Darby SA, ed. Clinical Anatomy of the Spine, Spinal Cord, and ANS. 3rd ed. St. Louis, MO: Elsevier Mosby; 2014: 566-85. Overall, the neck has lost some mobility in exchange for more sturdiness.
- Adulthood. The fully developed cervical spine has reached its peak in terms of providing an optimal balancing act of supporting the head and protecting the spinal cord while still enabling a high degree of mobility. However, at this point it has also started to exhibit at least some degeneration. Throughout adulthood, the cervical discs gradually lose hydration, facet joints lose more and more protective cartilage, and the cervical spine tends to drift forward while the height of the neck (and thus head) tends to go down.
See Facet Joint Anatomy Animation
By age 70, most cervical spines show significant degeneration visible on X-rays as well as on MRI imaging, even though few people feel or notice any symptoms.2Teraguchi M, Yoshimura N, Hashizume H, et al. Prevalence and distribution of intervertebral disc degeneration over the entire spine in a population-based cohort: the Wakayama Spine Study. Osteoarthr Cartil. 2014; 22(1):104-10
When Spinal Degeneration is Serious
Numbness and loss of balance due to spinal degeneration warrants prompt medical attention.
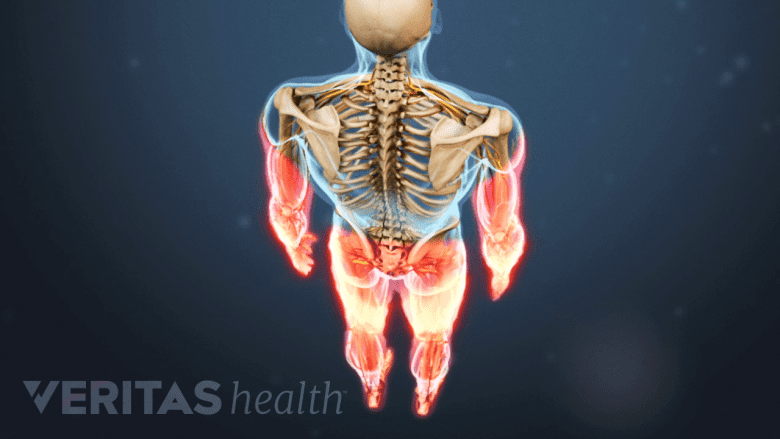
In some cases, spinal degeneration can progress to the point of causing a nerve root to become pinched and/or inflamed, which can cause cervical radiculopathy symptoms to radiate down into the arm, such as severe pain, pins-and-needles tingling, numbness, and/or weakness. It is also possible for spinal degeneration to encroach into the main aspect of the spinal canal and push against the spinal cord, which could lead to myelopathy symptoms such as difficulty with coordination, balance, walking, bowel and bladder function, and/or pain that shoots down the back or leg.
If cervical radiculopathy or myelopathy symptoms are not addressed by a doctor, it is possible for permanent nerve damage to occur.
- 1 Cramer GD, Y SW. Unique anatomic features of the pediatric spine. In: Cramer GD, Darby SA, ed. Clinical Anatomy of the Spine, Spinal Cord, and ANS. 3rd ed. St. Louis, MO: Elsevier Mosby; 2014: 566-85.
- 2 Teraguchi M, Yoshimura N, Hashizume H, et al. Prevalence and distribution of intervertebral disc degeneration over the entire spine in a population-based cohort: the Wakayama Spine Study. Osteoarthr Cartil. 2014; 22(1):104-10

