With appropriate treatment, mild sacroiliac (SI) joint pain may resolve within a few days to weeks, while more severe cases may take several months for complete recovery.
If left untreated, SI joint pain can become chronic and increase in severity, affecting your ability to perform daily activities.1Baronio M, Sadia H, Paolacci S, et al. Etiopathogenesis of sacroiliitis: implication for assessment and management. Korean J Pain. 2022;33(4):294-304. http://doi.org/10.3344/kjp.2020.33.4.294
Recovery from SI joint pain can vary depending on the underlying cause of SI joint dysfunction. Research indicates that up to 95% of patients with SI joint pain respond well to non-surgical treatments with significant pain reduction within 1 to 3 months.2Zelle BA, Gruen GS, Brown S, George S. Sacroiliiac joint dysfunction: evaluation and management. Clin J Pain. 2005; 21:446-355. https://pubmed.ncbi.nlm.nih.gov/16093751
How can I relieve SI joint pain quickly?
Over-the-counter (OTC) pain medications can help reduce inflammation.
When SI joint pain starts, the following methods can help control the symptoms in the short term:
- Take rest. Resting for a day or two and avoiding activities that increase the pain may help relieve mild to moderate SI joint inflammation. During this time, cold therapy followed by heat therapy may be tried to help reduce inflammation and alleviate pain. It is advisable to consult a physician if the pain does not resolve within this period.
- Try medication that reduces inflammation. Over-the-counter (OTC) pain medications, such as non-steroidal anti-inflammatory drugs (NSAIDs), can help reduce inflammation and temporarily relieve SI joint pain.3Rashbaum RF, Ohnmeiss DD, Lindley EM, Kitchel SH, Patel VV. Sacroiliac Joint Pain and Its Treatment. Clin Spine Surg. 2016;29(2):42-48. http://doi.org/10.1097/BSD.0000000000000359
- It is important to note that some NSAIDs may not be suitable for everyone due to the potential risk of gastric irritation and cardiac problems. To avoid these risks, consulting a physician before taking these medications is advisable.
- Ask your doctor about medication that relaxes muscles. When the muscles around the SI joint become tense or spasm, they can put pressure on the joint and exacerbate pain. Muscle relaxants like cyclobenzaprine and baclofen may be prescribed to help relax the muscles around the SI joint and alleviate pain.4Falowski S, Sayed D, Pope J, Patterson D, Fishman M, Gupta M, Mehta P. A Review and Algorithm in the Diagnosis and Treatment of Sacroiliac Joint Pain. J Pain Res. 2020;13:3337-3348. http://doi.org/10.2147/JPR.S279390
- Modify your everyday activities. Alterations to daily activities can help take the pressure off the SI joints. Essential lifestyle changes that can help manage symptoms of SI joint pain include5Lee A, Gupta M, Boyinepally K, Stokey PJ, Ebraheim NA. Sacroiliitis: A Review on Anatomy, Diagnosis and Treatment. Advances in Orthopedics. 2022. http://doi.org/10.1155/2022/3283296:
- Making ergonomic changes at the workplace, such as using a standing desk or adjusting the height of the chair, can help improve posture and decrease painful symptoms.
- Staying active, taking regular walking breaks between work, and avoiding sitting or standing for too long to promote blood flow and circulation which can help reduce stiffness and reduce pain.
- Using orthotics and supportive shoes helps improve the alignment of the foot and reduce the strain on the SI joint.6O’Leary CB, Cahill CR, Robinson AW, Barnes MJ, Hong J. A systematic review: The effects of podiatrical deviations on nonspecific chronic low back pain. Journal of Back and Musculoskeletal Rehabilitation. 2013;26(2):117-123. http://doi.org/10.3233/BMR-130367
- Try therapeutic exercises. Therapeutic exercise and physical therapy help improve the strength and flexibility of the muscles surrounding the SI joint, which can help alleviate pain and prevent future flare-ups.3Rashbaum RF, Ohnmeiss DD, Lindley EM, Kitchel SH, Patel VV. Sacroiliac Joint Pain and Its Treatment. Clin Spine Surg. 2016;29(2):42-48. http://doi.org/10.1097/BSD.0000000000000359
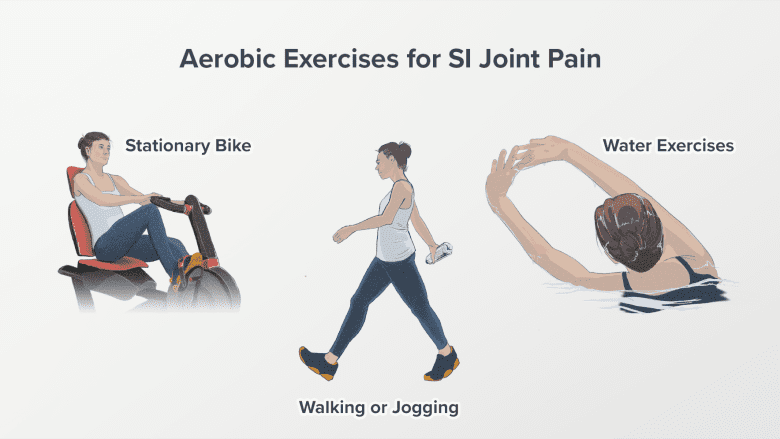
Aerobic exercises can help improve muscle strength and blood flow in the lower back.
-
- It is recommended that a doctor or physical therapist familiar with the patient’s specific needs is consulted before starting a new exercise program. A prior consultation ensures that a new exercise will not cause further exacerbation of pain.
- Sometimes, taking an NSAID or muscle relaxant may be recommended to help control acute pain before starting a physical therapy program.
- Consider therapeutic massage. Massage therapy can help relax the soft tissues around the SI joint, improve blood flow to the area, and promote healing in the joint area. Massages can be self-administered by the patient or delivered by a licensed massage therapist and can involve a few different techniques:
- Neuromuscular massage: applying firm, sustained pressure to the affected area using your fingers and moving in a circular motion. This maneuver helps to release tension in the surrounding muscles and connective tissue, thereby reducing the pressure on the SI joint.7Romanowski MW, Spiritovic M, Rutkowski R, Dudek A, Samborski W, Straburzynska-Lupa A. Comparison of Deep Tissue Massage and Therapeutic Massage for Lower Back Pain, Disease Activity, and Functional Capacity of Ankylosing Spondylitis Patients: A Randomized Clinical Pilot Study. Evidence-Based Complementary and Alternative Medicine. 2017;9894128. https://doi.org/10.1155/2017/9894128
- Deep tissue massage: applying deep, firm pressure along specific energy lines in the body. This massage is typically administered by a licensed therapist and provides deep tissue relaxation.
It is important to note that SI joint pain that occurs after an accident or trauma or develops in tandem with other symptoms like fever or loss of appetite may indicate a serious medical condition and requires prompt medical evaluation. Additionally, symptoms such as leg weakness, bowel and/or bladder dysfunction, or sexual dysfunction also warrant immediate medical attention.
Are injection treatments effective in relieving SI joint pain?

Injections may be effective at relieving SI joint pain.
Steroid, local anesthetic,8Wu L, Tafti D, Varacallo M. Sacroiliac Joint Injection. [Updated 2022 Sep 7]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513245/ or prolotherapy injections9Hoffman MD, Agnish V. Functional outcome from sacroiliac joint prolotherapy in patients with sacroiliac joint instability. Complementary Therapies in Medicine. 2018;37:64-68. http://doi.org/10.1016/j.ctim.2018.01.014 may be considered for SI joint pain that does not respond to the treatments listed above. The duration of pain relief from SI joint injections varies among patients.
Research indicates that a majority of patients may experience up to a 70% reduction in pain in the weeks following injection treatment but may require additional injections after 6 months.10Kim WM, Lee HG, Jeong CW, Kim CM, Yoon MH. A Randomized Controlled Trial of Intra-Articular Prolotherapy Versus Steroid Injection for Sacroiliac Joint Pain. The Journal of Alternative and Complementary Medicine. 2010;16(12):1285-1290.
- Steroid and anesthetic injections reduce the activity of the immune system to decrease the production of inflammatory cells in the body.
- Prolotherapy injections involve injecting small amounts of a medicated solution into the target musculoskeletal tissue(s) over a period of several weeks with the goal of inducing tissue regeneration, promoting healing, and reducing pain.11Rabago D, Nourani B. Prolotherapy for Osteoarthritis and Tendinopathy: a Descriptive Review. Curr Rheumatol Rep. 2017;19(6):34. http://doi.org/10.1007/s11926-017-0659-3,12Bae G, Kim S, Lee S, Lee WY, Lim Y. Prolotherapy for the patients with chronic musculoskeletal pain: systematic review and meta-analysis. Anesth Pain Med (Seoul). 2021;16(1):81-95. http://doi.org/10.17085/apm.20078
- Platelet-rich plasma (PRP) injections involve injecting a concentration of a patient’s own platelets from their blood to accelerate the healing of injured joints, tendons, and muscles.13Singla V, Batra YK, Bharti N, Goni VG, Marwaha N. Steroid vs. Platelet-Rich Plasma in Ultrasound-Guided Sacroiliac Joint Injection for Chronic Low Back Pain. Pain Pract. 2017;17(6):782-791. http://doi.org/10.1111/papr.12526
- Radiofrequency ablation (RFA) is a type of injection that involves heating a part of the pain-transmitting nerve with a radiofrequency needle to create a heat lesion. Preventing the nerve from sending pain to the brain.14Schmidt PC, Pino CA, Vorenkamp KE. Sacroiliac Joint Radiofrequency Ablation with a Multilesion Probe: A Case Series of 60 patients. Anesthesia & Analgesia. 2014;119(2):460-462. http://doi.org/10.1213/ANE.0000000000000282
While PRP injections and RFA may be considered for the treatment of SI joint pain, steroid, local anesthetic, and prolotherapy injections are the most commonly used injection treatment.
Injections are minimally invasive and are usually considered a safe and low-risk procedure. However, as with any injection treatment, there is always a chance of developing side effects or potential complications, such as allergic reactions, nerve damage, bleeding, or infection, which must be discussed in detail with the physician before considering these treatments.
What happens if SI joint pain is left untreated?

The SI joint can become inflamed from overuse, leading to joint changes and painful symptoms.
If left untreated, some cases of SI joint dysfunction may worsen over time.15Raj MA, Ampat G, Varacallo M. Sacroiliac Joint Pain. [Updated 2022 Sep 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470409/ The progression of SI joint dysfunction varies from one individual, and while the pain may resolve for some people, others may experience one or more of the following:
- Chronic pain. Untreated SI joint pay may become chronic, leading to persistent discomfort when performing physical activities.1Baronio M, Sadia H, Paolacci S, et al. Etiopathogenesis of sacroiliitis: implication for assessment and management. Korean J Pain. 2022;33(4):294-304. http://doi.org/10.3344/kjp.2020.33.4.294
- Degenerative changes. Over time, degenerative changes may occur in the joint, such as the development of bone spurs or arthritis. These changes can lead to worsening pain and decreased mobility.1Baronio M, Sadia H, Paolacci S, et al. Etiopathogenesis of sacroiliitis: implication for assessment and management. Korean J Pain. 2022;33(4):294-304. http://doi.org/10.3344/kjp.2020.33.4.294
- Compensatory injuries. Individuals with one-sided SI joint pain tend to naturally alter their posture or movement patterns to compensate for pain and dysfunction. This type of natural compensation can cause increased stress and strain on the opposite hip and lead to additional injuries or muscle imbalances.16Kao MC, Chuang CW, Hung SK, Pan PT. Diagnosis and interventional pain management options for sacroiliac joint pain. Tzu Chi Medical Journal. 2019;31(4):207-210.
Addressing the underlying cause of SI joint pain early through appropriate treatment can help prevent the progression of the condition and improve the quality of life.
Do I need surgery for SI joint pain?

Metal implants are used to fuse the SI joint.
Surgery for SI joint dysfunction is rare and typically considered when non-surgical treatments have failed to provide relief, and the patient experiences significant pain and limited mobility that interferes with daily activities.3Rashbaum RF, Ohnmeiss DD, Lindley EM, Kitchel SH, Patel VV. Sacroiliac Joint Pain and Its Treatment. Clin Spine Surg. 2016;29(2):42-48. http://doi.org/10.1097/BSD.0000000000000359 A surgeon specializing in musculoskeletal conditions can advise if surgery is an option for SI joint pain and the potential benefits and risks associated with the procedure.
SI joint fusion surgery may be performed using minimally invasive techniques but generally involves making a larger incision near the SI joint to remove damaged cartilage or tissues before placing bone grafts or metal implants to fuse the two bones that make up the SI joint.3Rashbaum RF, Ohnmeiss DD, Lindley EM, Kitchel SH, Patel VV. Sacroiliac Joint Pain and Its Treatment. Clin Spine Surg. 2016;29(2):42-48. http://doi.org/10.1097/BSD.0000000000000359 The decision to use a minimally invasive technique depends on the patient’s underlying condition and the experience and skill of the treating surgeon.17Cohen SP, Chen Y, Neufeld NJ. Sacroiliac joint pain: a comprehensive review of epidemiology, diagnosis and treatment. Expert Rev Neurother. 2013;13(1):99-116. http://doi.org/10.1586/ern.12.148
Learn more:
- 1 Baronio M, Sadia H, Paolacci S, et al. Etiopathogenesis of sacroiliitis: implication for assessment and management. Korean J Pain. 2022;33(4):294-304. http://doi.org/10.3344/kjp.2020.33.4.294
- 2 Zelle BA, Gruen GS, Brown S, George S. Sacroiliiac joint dysfunction: evaluation and management. Clin J Pain. 2005; 21:446-355. https://pubmed.ncbi.nlm.nih.gov/16093751
- 3 Rashbaum RF, Ohnmeiss DD, Lindley EM, Kitchel SH, Patel VV. Sacroiliac Joint Pain and Its Treatment. Clin Spine Surg. 2016;29(2):42-48. http://doi.org/10.1097/BSD.0000000000000359
- 4 Falowski S, Sayed D, Pope J, Patterson D, Fishman M, Gupta M, Mehta P. A Review and Algorithm in the Diagnosis and Treatment of Sacroiliac Joint Pain. J Pain Res. 2020;13:3337-3348. http://doi.org/10.2147/JPR.S279390
- 5 Lee A, Gupta M, Boyinepally K, Stokey PJ, Ebraheim NA. Sacroiliitis: A Review on Anatomy, Diagnosis and Treatment. Advances in Orthopedics. 2022. http://doi.org/10.1155/2022/3283296
- 6 O’Leary CB, Cahill CR, Robinson AW, Barnes MJ, Hong J. A systematic review: The effects of podiatrical deviations on nonspecific chronic low back pain. Journal of Back and Musculoskeletal Rehabilitation. 2013;26(2):117-123. http://doi.org/10.3233/BMR-130367
- 7 Romanowski MW, Spiritovic M, Rutkowski R, Dudek A, Samborski W, Straburzynska-Lupa A. Comparison of Deep Tissue Massage and Therapeutic Massage for Lower Back Pain, Disease Activity, and Functional Capacity of Ankylosing Spondylitis Patients: A Randomized Clinical Pilot Study. Evidence-Based Complementary and Alternative Medicine. 2017;9894128. https://doi.org/10.1155/2017/9894128
- 8 Wu L, Tafti D, Varacallo M. Sacroiliac Joint Injection. [Updated 2022 Sep 7]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513245/
- 9 Hoffman MD, Agnish V. Functional outcome from sacroiliac joint prolotherapy in patients with sacroiliac joint instability. Complementary Therapies in Medicine. 2018;37:64-68. http://doi.org/10.1016/j.ctim.2018.01.014
- 10 Kim WM, Lee HG, Jeong CW, Kim CM, Yoon MH. A Randomized Controlled Trial of Intra-Articular Prolotherapy Versus Steroid Injection for Sacroiliac Joint Pain. The Journal of Alternative and Complementary Medicine. 2010;16(12):1285-1290.
- 11 Rabago D, Nourani B. Prolotherapy for Osteoarthritis and Tendinopathy: a Descriptive Review. Curr Rheumatol Rep. 2017;19(6):34. http://doi.org/10.1007/s11926-017-0659-3
- 12 Bae G, Kim S, Lee S, Lee WY, Lim Y. Prolotherapy for the patients with chronic musculoskeletal pain: systematic review and meta-analysis. Anesth Pain Med (Seoul). 2021;16(1):81-95. http://doi.org/10.17085/apm.20078
- 13 Singla V, Batra YK, Bharti N, Goni VG, Marwaha N. Steroid vs. Platelet-Rich Plasma in Ultrasound-Guided Sacroiliac Joint Injection for Chronic Low Back Pain. Pain Pract. 2017;17(6):782-791. http://doi.org/10.1111/papr.12526
- 14 Schmidt PC, Pino CA, Vorenkamp KE. Sacroiliac Joint Radiofrequency Ablation with a Multilesion Probe: A Case Series of 60 patients. Anesthesia & Analgesia. 2014;119(2):460-462. http://doi.org/10.1213/ANE.0000000000000282
- 15 Raj MA, Ampat G, Varacallo M. Sacroiliac Joint Pain. [Updated 2022 Sep 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470409/
- 16 Kao MC, Chuang CW, Hung SK, Pan PT. Diagnosis and interventional pain management options for sacroiliac joint pain. Tzu Chi Medical Journal. 2019;31(4):207-210.
- 17 Cohen SP, Chen Y, Neufeld NJ. Sacroiliac joint pain: a comprehensive review of epidemiology, diagnosis and treatment. Expert Rev Neurother. 2013;13(1):99-116. http://doi.org/10.1586/ern.12.148

